An international research team has discovered that the jumonji domain-containing 6 (JMJD6) gene plays a critical role in neuroblastoma tumorigenesis. In addition, in work that opens up a potential new target for the treatment of neuroblastoma, they showed that when JMJD6’s expression was reduced, neuroblastoma cell proliferation and survival in vitro and tumor progression in mice were decreased.
The work was published in Nature Communications in a paper entitled, “JMJD6 is a tumorigenic factor and therapeutic target in neuroblastoma.”
Neuroblastoma accounts for 15% of all childhood cancer deaths. The most common genetic change in human neuroblastoma tissues is a gain of the chromosomal region 17q. However, the particular genes at chromosome 17q that are important for neuroblastoma tumorigenesis have eluded researchers.
Tao Liu, Ph.D., associate professor and group leader, and his research team from the Children’s Cancer Institute Australia in Sydney, identified JMJD6 from a tumor database of 209 patients, finding the gene active in more than one in four patients with the aggressive form of neuroblastoma. They did this through the analysis of matched human neuroblastoma tissue array-CGH (comparative genomic hybridization) and gene expression datasets.
The authors found that “the JMJD6 gene is commonly gained in human neuroblastoma tissues, and that a high level of JMJD6 expression independently predicts poor patient prognosis.”
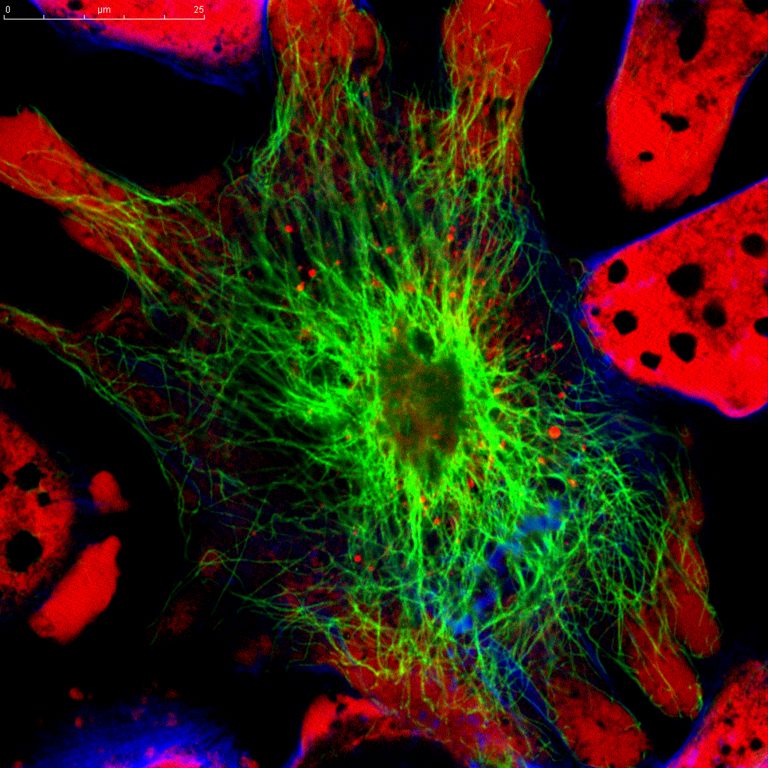
The team found that JMJD6, a dual arginine demethylase and lysyl hydroxylase of histone and nonhistone proteins, activates gene transcription. They showed that JMJD6 forms protein complexes with N-Myc and BRD4, and is important for E2F2, N-Myc, and c-Myc transcription. When they decreased the expression of JMJD6, they showed several promising results in mice, including a reduction in neuroblastoma cell proliferation and survival in vitro and tumor progression in mice.
The research team, including first author Matthew Wong, PhD, a research officer in the Liu lab of at the Children’s Cancer Institute, used a combination therapy—super-enhancer and histone deacetylase inhibitors—targeting JMJD6 gene expression in a mouse model of the disease. The researchers found that after three weeks of drug combination treatment, neuroblastoma tumor size was reduced by 80% compared to the control. According to Liu, similar drugs to the ones used in their experiments are currently in clinical trials for other cancers, making it more likely that this particular treatment strategy will be available for clinical trials of neuroblastoma.
The most exciting part of the study, according to Hong-Xi Xu, Ph.D., professor and dean at the Shanghai University of Traditional Chinese Medicine and author on the paper, was that “the gene critical for the tumorigenesis of chromosome 17q-gained neuroblastoma has been identified, and a novel therapy targeting JMJD6 has been validated in the laboratory.” Xu adds that “discoveries from this study pave the way for further development of more clinically applicable therapies in chromosome 17q-gained neuroblastoma patients.”













