It may be possible to reawaken a patient’s own immune response against a bladder tumor using immunotherapy, according to a recent study by scientists from Barts Cancer Institute in London, Queen Mary University of London, and HistoGeneX in Belgium, which is a laboratory focused on tissue pathology and genomics. Their study was reported in the most recent issue of Nature Medicine.
Bladder cancer is the ninth most common cancer in the world, with 430,000 new cases diagnosed in 2012. Approximately 80,000 new cases and 18,000 deaths occur each year in the US alone due to this disease. Approximately 25% of patients will have muscle-invasive disease and either present with or later develop metastases. For these patients, the median survival with first-line, multiagent chemotherapy is only about 15 months. While second-line chemotherapy has a role, checkpoint inhibitor immunotherapy offers another option for patients progressing after initial systemic therapy.
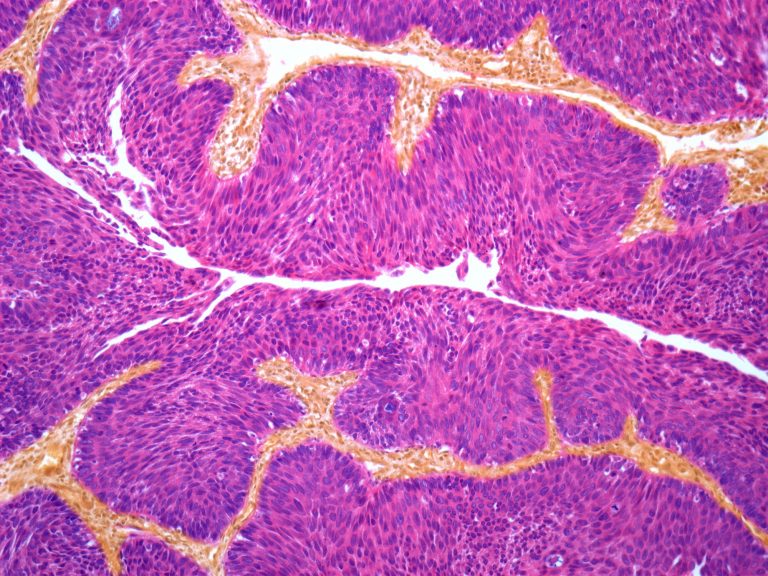
This report describes single-arm phase II study, investigating two cycles of atezolizumab, a cancer immunotherapy, before cystectomy in 95 patients with muscle-invasive urothelial cancer (ClinicalTrials.gov identifier: NCT02662309). The primary endpoint was pathological complete response, with secondary endpoints focused on safety, relapse-free survival and biomarker analysis. In the study, 95 patients with invasive bladder cancer received two cycles of anti-PDL1 before their cystectomy (partial or total removal of the bladder) was performed. The initial bladder biopsies collected for diagnosis, and prior to anti-PDL1 therapy, were compared with the bladder resections. Examination of the resections revealed that the tumor had completely disappeared in 31% of the cases.
Pathological complete response was the primary endpoint. Secondary endpoints focused on safety, relapse-free survival and biomarker analysis. The pathological complete response rate was 31% (95% confidence interval: 21–41%), achieving the primary efficacy endpoint. Baseline biomarkers showed that the presence of preexisting activated T cells was more prominent than expected and correlated with outcome. Other established biomarkers, such as tumor mutational burden, did not predict outcome, differentiating this from the metastatic setting. Dynamic changes to gene expression signatures and protein biomarkers occurred with therapy, whereas changes in DNA alterations with treatment were uncommon.
These results demonstrated that the quantity and quality of the immune cell infiltration of the initial biopsies was strongly predictive of a good response to the treatment. However, non-responders often showed very specific defects that prevented successful immunotherapy. “We are currently mapping out all these response and resistance mechanisms,” said pathologist Mark Kockx, a co-author of the study and co-founder of HistoGeneX.
Other studies have reported that antibodies targeting PD-1 or its ligand 1 PD-L1 such as atezolizumab, have great efficacy in some metastatic urothelial cancers. And there are biomarkers being studied to develop which of these cancers are responsive. Neoadjuvant use of PD-1 and PD-L1 antibodies is associated with pathological complete response in a spectrum of tumors, including urothelial cancer.
Based in this study, the researchers assume that in the future it will be possible to predict which tumors will respond to immune therapy, therefore minimizing the need for bladder resection.













