Choosing the best treatments for cancer patients may rely on both medical images as well as genetic and cellular analysis, according to researchers from the Translational Genomics Research Institute (TGen), an affiliate of City of Hope, and their collaborators. This combination of tests could help surgeons best decide how much tissue to remove, the dosage and frequency of radiation therapy, and which drugs are best suited for a particular patient.
Published in PLOS ONE, this paper reinforces the critical role of the tumor microenvironment (TMV), which comprises cells both in and surrounding a tumor. Research on the TMV has rapidly advanced in recent years, but it is still unclear which are the critical markers cancer doctors should pay the most attention to.
“This study is a bridge between genetic sequencing, single-cell analysis and high-resolution medical imaging,” said Michael Berens, professor and director of TGen’s Cancer and Cell Biology Division, head of the institute’s Glioma Research Lab, and one of the study’s lead authors. “By literally focusing on how tumors look on the outside, as well as spelling out their DNA cell characteristics on the inside, we believe we can provide physicians, oncologists, radiologists, surgeons and others with timely information about how to best attack each patient’s cancer.”
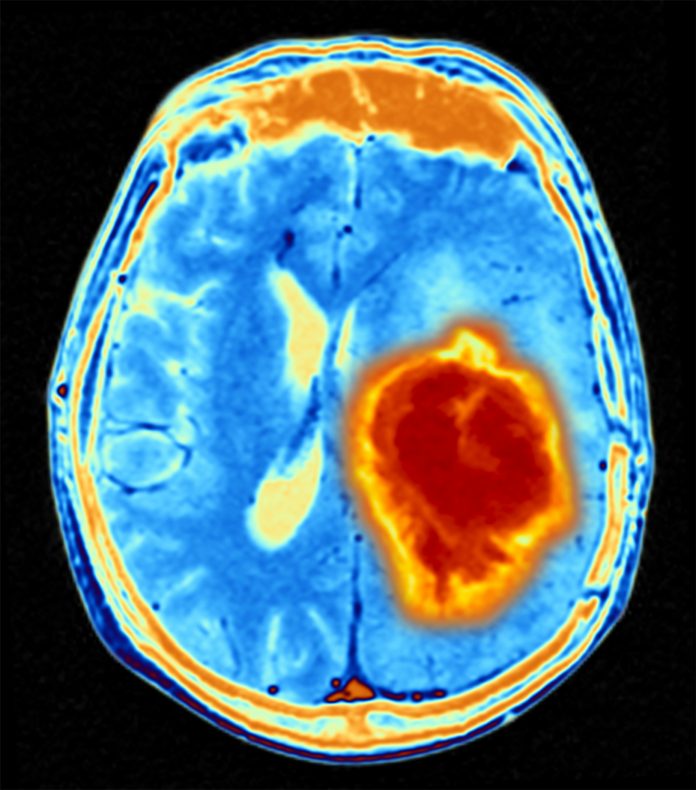
In this report Berens and his collaborators correlated the genetic and protein fingerprints of brain cancer cells with how those cells, and surrounding cells looked, using MRI (magnetic resonance imaging), a test routinely performed as soon as brain cancer is suspected.
TGen’s partnering investigators at General Electric Global Research Center deployed a novel imaging tool, which they developed over the past decade together with GE Healthcare. This tool is called “Cell Dive,” and it uses multiplexed immunofluorescence imaging (MxIF). This process can repeatedly stain tumor samples with antibodies attached to fluorescent dyes. In an iterative process of staining and imaging, the method allows cell level quantification of over 60 cell biomarkers in a single sample.
For this study, the researchers analyzed more than 100,000 cells in brain tumor cases, using MxIF to uncover differences between two types of brain tumors based on mutations in the gene IDH1. Based on MxIF analysis, 85,767 cells (glioma cases) and 56,304 cells (glioblastoma multiforme’s cases) were used to generate cell-level data for 24 biomarkers.
“Using this platform, we can visualize and analyze various cell types and cell states present in the tumor tissue as well as how they interact with each other and their microenvironment,” said Anup Sood, a senior scientist at GE Global Research, and also a lead author of the study.
“The resolution of MRI can’t ‘see’ individual cell differences. But we were able to find evidence for correlations between genetic and cellular changes. We can see the consequences of specific genetic changes in brain cancer tumors that show up on a medical image,” Berens said
This type of analysis is especially needed for brain cancer patients, whose fast-growing tumors are among the most difficult to diagnose, treat, remove and monitor. Because of the way brain tumors infiltrate surrounding healthy brain tissue, it is difficult for surgeons to remove all of the cancer without causing potentially catastrophic damage to a patient’s memory and ability to function. And because of a matrix of tiny blood vessels that surround and protect the brain, only the smallest molecules can enter, limiting the types of drugs that could help shrink brain tumors.
Adding to the difficulty is the fact that each patient’s brain tumor cells are different. Even the individual cancer cells within the tumor can vary.
Fiona Ginty, a GE senior scientist and the study’s senior author, added: “The more cell-level data we analyze, the more we learn about tumor biology, cell-to-cell interactions, immune response and how tumors progress. Further, with the integration of cellular, medical imaging and genomic data, we gain a more holistic understanding of why certain tumor types progress more rapidly, and others are more slow-growing, and ultimately which drugs a patient may respond to.”













