While the bulk of COVID-19 testing relies on reverse transcription polymerase chain reaction (RT-PCR) technology, there has been significant evidence to show that tests based on this method are far from the standard one would typically expect from a clinical diagnostic as many have called into question both the sensitivity and specificity of the RT-PCR tests. Additionally, shortages of reagents and trained personnel to run the tests can create a bottleneck in generating timely testing results.
Now, an alternative technology called localized surface plasmon resonance (LSPR) sensing, could help provide a lift to COVID-19 testing, according to researchers based at ETH Zurich. According to new findings from the group, when LPSR is tasked with detecting COVID-19 RNA, its demonstrates a high degree of accuracy and sensitivity—and speediness.
The researchers presented a proof-of-concept study that appeared April 13 in ACS Nano. The study, titled, “Dual-Functional Plasmonic Photothermal Biosensors for Highly Accurate Severe Acute Respiratory Syndrome Coronavirus 2 Detection,” describes a dual-functional plasmonic photothermal (PPT)-enhanced LSPR biosensing system.
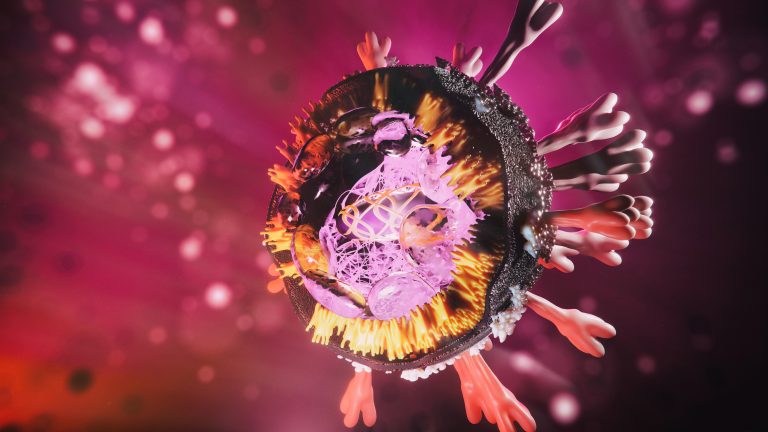
Like other LPSR systems, the ETH researchers’ system detects interactions between molecules on the surface of a constructed metallic nanostructure, and it registers interactions as a local change in refractive index. The ETH researchers’ system, however, has the distinction of incorporating DNA probes that recognize specific SARS-CoV-2 RNA sequences.
The probes are attached to gold nanoparticles—actually, two-dimensional gold nanoislands, or AuNIs—and they detect SARS-CoV-2 RNA through nucleic acid hybridization. Essentially, the DNA probes attach to complementary viral RNA like a zipper being closed.
“For better sensing performance, the thermoplasmonic heat is generated on the same chip-based AuNIs when illuminated at their plasmonic resonance frequency,” the article’s authors noted. “The localized PPT heat is capable to elevate the in situ hybridization temperature and facilitate the accurate discrimination of two similar gene sequences.”
In other words, the ETH Zurich researchers (led by Jing Wang, PhD) used a laser to heat up the nanoparticles, making it more difficult for imperfectly matched sequences to remain attached, reducing false-positive results. For example, a nucleic acid “zipper” missing a couple of teeth—indicating a partial mismatch—would unzip under these conditions. In this way, the researchers could discriminate between SARS-CoV-2 and its close relative, SARS-CoV-1.
“Our dual-functional LSPR biosensor,” the article’s authors declared, “exhibits a high sensitivity toward the selected SARS-CoV-2 sequences with a lower detection limit down to the concentration of 0.22 pM and allows precise detection of the specific target in a multigene mixture.”
The assay detected amounts of viral RNA below those present in respiratory swabs in a matter of minutes. “Under the outbreak background of COVID-19,” the authors concluded, “this proposed dual-functional LSPR biosensor can provide a reliable and easy-to-implement diagnosis platform to improve the diagnostic accuracy in clinical tests and relieve the pressure on PCR-based tests.”
Before that happens, the system will need to be tested on intact viral RNA from patient samples. Also, certain practical limitations of SPR systems will need to be addressed. Such limitations were discussed in an article (“The Role of Surface Plasmon Resonance in Clinical Laboratories”) that appeared last year in Clinical Laboratory News:
“[The instrumentation is expensive, ranging anywhere from $50,000 to $300,000 depending on the throughput or number of channels in the instrument. In addition, only a handful of companies make the instruments. Several firms supply the instruments, and these companies primarily design and market their instruments for academic and pharmaceutical laboratories. Vendors’ focus on research and pharmaceutical applications partly explains why clinical laboratorians are not very familiar with the instruments and may have the perception that the technique is too complex for their needs.”
The same article also noted that SPR technology has several advantages: “It can be automated, requires few biological reagents for method development, and generates results in just a few minutes.” In these respects, SPR may outshine other RT-PCR alternatives. For example, computed tomography scanning and culturing, does not provide quick or real-time results.
The impetus to overcome LSPR’s difficulties may come from the desire to bring the coronavirus under control. Health experts agree that expanded testing is crucial for controlling the spread of COVID-19. However, testing in many countries, including the United States, has lagged because of limited supplies of some reagents and a backlog of samples awaiting available PCR machines and laboratory personnel. In addition, RT-PCR methods have been known to produce false-negative and -positive test results.











