Over the weekend, the FDA granted Regeneron Pharmaceuticals an emergency use authorization (EUA) for its two-antibody “cocktail” REGEN-COV2 (formerly REGN-COV2) as a treatment for adults and youths ages 12 years and older with mild-to-moderate COVID-19.
The EUA allows for the distribution and emergency use of REGEN-COV2, which consists of casirivimab (formerly known as REGN10933) and imdevimab (formerly REGN10987).
REGEN-COV2 is the second antibody therapy against COVID-19 authorized for emergency use in nearly two weeks; on November 10, the FDA granted an EUA to Eli Lilly’s bamlanivimab (LY-CoV555), with a nearly identical indication and restrictions on its use.
Before patients can be treated with REGEN-COV2 under the EUA, they must weigh at least 40 kilograms (about 88 pounds) and be deemed at high risk for progressing to severe COVID-19 and/or hospitalization. That high-risk category includes adults who are ages 65 or older, or who have chronic medical conditions.
“This FDA Emergency Use Authorization is an important step in the fight against COVID-19, as high-risk patients in the United States will have access to a promising therapy early in the course of their infection,” Regeneron president and CEO Leonard S. Schleifer, MD, PhD, said in a statement issued by his company.
Last month, soon after testing positive for COVID-19, President Donald Trump began his treatment regimen for the virus with REGEN-COV2 before adding Gilead Sciences’ remdesivir, marketed in the United States as Veklury and other treatments.
President Trump “received a single 8 g dose” of REGEN-COV2, Conley wrote in a letter made public by the White House on October 2.
That is a higher dose than the dosage recommended by the EUA, which is 2.4 g (2,400 mg)—consisting of 1.2 g (1,200 mg) of casirivimab and 1.2 g of imdevimab, administered as a single intravenous infusion. The dosage was changed this fall after data from a clinical trial in ambulatory patients found no significant difference in efficacy between the doses.
Washington also has a financial stake in REGEN-COV2: The federal government has committed to Regeneron up to $617.7 million-plus toward REGEN-COV2 through “Operation Warp Speed”—the Trump administration’s effort to fund development, manufacturing, and distribution of COVID-19 drugs and vaccines. That commitment includes a $450.3 million award to demonstrate large-scale manufacturing of the antibody cocktail.
Up to 300,000 patients
Regeneron said it expects to have REGEN-COV2 treatment doses ready for approximately 80,000 patients by the end of November, rising to approximately 200,000 by the first week of January, and approximately 300,000 patients total by the end of January 2021.
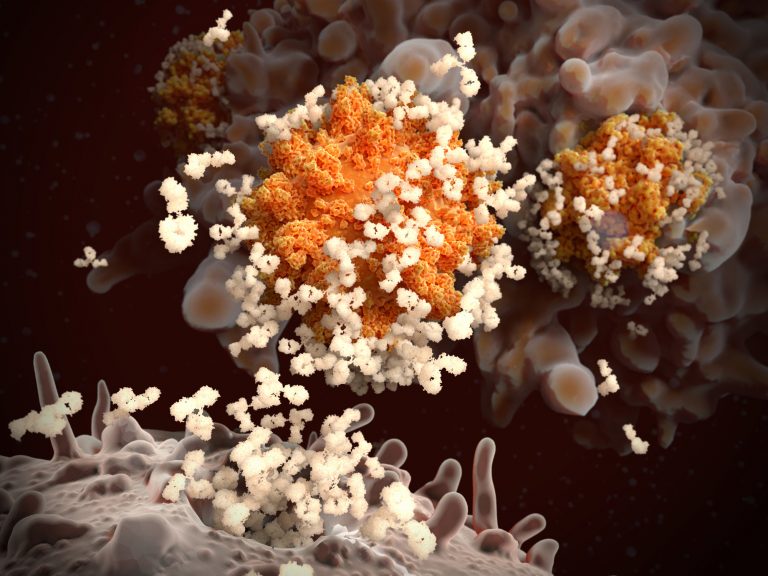
Both casirivimab and imdevimab are designed to bind non-competitively to the receptor-binding domain (RBD) of SARS-CoV-2’s spike protein. According to a paper published August 21 in Science, casirivimab targets the spike-like loop region on one edge of the ACE2 interface. The fragment antigen-binding region of casirivimab binds the RBD from the top, where it collides with ACE2, while imdevimab only binds to the front or the lower left side of the RBD.
“REGEN-COV2 is designed to mimic what a well-functioning immune system does by using very potent antibodies to neutralize the virus,” added George D. Yancopoulos, MD, PhD, Regeneron’s president and CSO.
The FDA based its EUA on positive clinical data announced by the company in September and October from the first 799 adults in the Phase II/III portion (NCT04425629) of an adaptive Phase I/II/III trial evaluating the safety, tolerability, and efficacy of REGEN-COV2 in ambulatory adult outpatients with COVID-19.
In its October announcement, Regeneron disclosed that it found no significant difference in efficacy between REGEN-COV2’s low dose of 2.4 g, and its high dose of 8 g—a finding that led to the change in dosage since President Trump took REGEN-COV2.
However, data from the 799 patients also showed that the antibody cocktail met its primary endpoint of significantly reducing viral load, and in the secondary endpoint of medically attended visits related to COVID-19, particularly hospitalizations and emergency room visits within 28 days after treatment.
For patients at high risk for disease progression, hospitalizations and emergency room visits occurred in 3% of casirivimab and imdevimab-treated patients on average compared to 9% in placebo-treated patients.
At-risk patient benefit
“This benefit was greatest in patients most at risk for poor outcomes due to high viral load, ineffective immune response at baseline or pre-existing risk factors,” Yancopoulos said. “We are encouraged that no variants resistant to the cocktail were identified in the clinical trial analyses to date, which is consistent with our preclinical findings.”
Of the 799 patients, 266 received a single intravenous infusion of 2.4 g casirivimab and imdevimab (1.2 g of each), 267 received 8 g casirivimab and imdevimab (4 g of each), and 266 received a placebo, within three days of obtaining a positive SARS-CoV-2 viral test. The randomized, double-blind trial had an estimated enrollment of 2,104 participants.
Casirivimab and imdevimab were the two most potent, non-competing, and virus-neutralizing antibodies selected from thousands produced through Regeneron’s monoclonal antibody discovery platform VelocImmune®, part of the company’s VelociSuite™ technologies. Regeneron has said it has produced two distinct antibody cocktails, an initial cocktail and a backup.
REGEN-COV2 is one of 20 “front runners” among more than 300 COVID-19 drug and vaccine candidates on GEN’s COVID-19 Drug & Vaccine Tracker.
“The FDA remains committed to advancing the nation’s public health during this unprecedented pandemic. Authorizing these monoclonal antibody therapies may help outpatients avoid hospitalization and alleviate the burden on our health care system,” FDA Commissioner Stephen M. Hahn, MD, said in a separate statement issued by the agency.
In granting the EUA, the FDA emphasized that REGEN-COV2 is not authorized for patients who are hospitalized due to COVID-19 or require oxygen therapy due to COVID-19, since no benefit to treatment with Regeneron’s antibody cocktail has been shown in those patients.
The FDA noted that monoclonal antibodies, such as casirivimab and imdevimab, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation.
Clinical setbacks
That appears to explain why, on October 26, the NIH’s National Institute of Allergy and Infectious Diseases (NIAID) halted the up-to-10,000 patient Phase III ACTIV-3 trial (NCT04501978) it was conducting to assess the safety and effectiveness of Lilly’s antibody therapy bamlanivimab compared with remdesivir and placebo in people who have been hospitalized with COVID-19.
Last month, Regeneron paused enrollment of patients requiring high-flow oxygen or mechanical ventilation in the Phase II/III portion (NCT04426695) of an adaptive Phase I/II/III trial assessing REGEN-COV2. Regeneron said it followed the recommendation of the trial’s independent data monitoring committee (IDMC) “based on a potential safety signal and an unfavorable risk/benefit profile at this time.” Regeneron has not disclosed the potential safety signal that triggered the enrollment pause.
The other two late-stage trials with which Regeneron is proceeding:
- A portion of the 15,000-patient open-label, Phase III RECOVERY (Randomized Evaluation of COVid-19 thERapY) trial (NCT04381936) that is examining the effectiveness of the cocktail plus standard of care in at least 2,000 hospitalized COVID-19 patients to be chosen at random in the U.K., and comparing that to another 2,000 patients who already receive standard of care alone.
- A Phase III trial (NCT04452318) designed to assess REGEN-COV2’s ability to prevent infection among uninfected people who have had close exposure to a COVID-19 patient, such as a patient’s housemate. The trial has an estimated enrollment of 2,000 participants.
REGEN-COV2 was granted its EUA a day after the FDA received a request from Pfizer and BioNTech for emergency authorization for their messenger RNA (mRNA)-based COVID-19 vaccine candidate BNT162b2. Moderna is expected to do likewise shortly for its mRNA-based vaccine candidate against the virus, mRNA-1273.
“We are also very encouraged by recently announced promising vaccine results; however, there remains a need to treat patients who develop COVID-19, especially as some may not have had access to or were not protected by vaccination,” Yancopoulos stated.













