A two-step positive-feedback circuit allows CAR-T cells to better discriminate solid tumor cancer targets, according to a new international study.
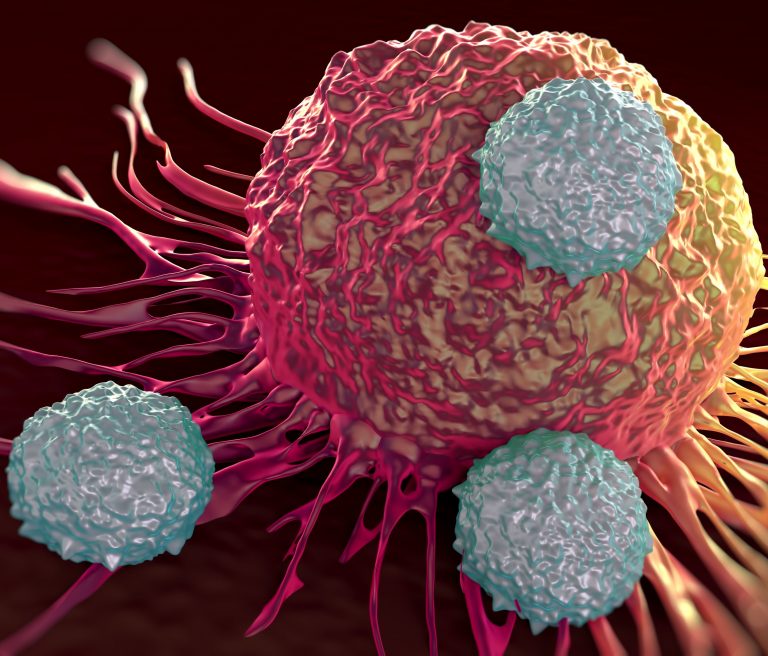
CAR-T cell therapy is a type of treatment in which a patient’s T cells are changed in the laboratory so they will attack cancer cells. CAR-T cell therapy is used to treat certain blood cancers, and it is being studied in the treatment of other types of cancer.
These treatments have been successfully used to treat patients with B cell lymphomas, and are currently undergoing clinical trials for the treatment of many other types of blood cancer. It has been one of the most significant recent advances in immunotherapies targeted at cancer. Recent studies have also reported using CAR-T therapy against solid tumors.
The new study demonstrates another approach of using CAR-T cells against solid tumors. The new strategy programs CAR-T cells so that they only kill cancer cells, leaving alone healthy cells that have the same marker protein as cancer cells.
The study, “T cell circuits that sense antigen density with an ultrasensitive threshold,” is published in Science and led by researchers from the University of California, San Francisco, and the University of Helsinki.
CAR-T cells may be less effective against solid tumors because they have to migrate into tumors and then survive long enough to kill all of the tumor cells. The cells and molecules surrounding tumors are often immunosuppressive, activating an immune checkpoint that causes the CAR-T cells to lose their activity.
Based on the ultrasensitive identification of HER2 cells, the new strategy uses a two-step identification process of HER2 positive cells. HER2 is a growth-promoting protein on the outside of all breast cells. Breast cancer cells with higher than normal levels of HER2 are called HER2-positive.
“Overexpressed tumor-associated antigens [for example, epidermal growth factor receptor (EGFR) and human epidermal growth factor receptor 2 (HER2)] are attractive targets for therapeutic T cells, but toxic ‘off-tumor’ cross-reaction with normal tissues that express low levels of target antigen can occur with chimeric antigen receptor (CAR)–T cells,” wrote the researchers. “Inspired by natural ultrasensitive response circuits, we engineered a two-step positive-feedback circuit that allows human cytotoxic T cells to discriminate targets on the basis of a sigmoidal antigen-density threshold.”
Kalle Saksela, PhD, professor of virology from the University of Helsinki explained further: “Our solution requires the preliminary identification of the surface structures associated with the cancer. When the preliminary recognition ability that induces the CAR construct is adjusted to require a binding affinity that is different from the affinity used by CAR to direct the killing of these cells, an extremely accurate ability to differentiate between cells based on the amount of target protein on their surface can be programmed in this two-step ‘circuit’ which controls the function of killer T cells.”
Further studies have already started to take flight. Postdoctoral researcher Anna Mäkelä, PhD, who works at Saksela’s laboratory, is coordinating a project funded by the Academy of Finland investigating the use of CAR-T cell therapy on various cancer types and their surface structures.
“We are very excited about these results, and we are currently developing the technique so that it could be used to treat ovarian cancer. As the work progresses, the aim is to apply the technique itself and the targeting molecules of CAR constructs even more broadly to malignant solid tumors. Our goal is to develop ‘multi-warhead missiles,’ against which cancer cells will find it difficult to develop resistance,” Mäkelä adds.
The researchers concluded, “Increasing HER2 density thus has cooperative effects on T cells—it increases both CAR expression and activation—leading to a sigmoidal response. T cells with this circuit show sharp discrimination between target cells expressing normal amounts of HER2 and cancer cells expressing 100 times as much HER2, both in vitro and in vivo.”













