New findings shed light on how tau protein development progresses through the brain. The study also provides insights into why some areas of the brain are more vulnerable to damage from tau than others. The results were published in Science Advances by researchers at Van Andel Institute and University of Pennsylvania. https://advances.sciencemag.org/content/7/24/eabg6677
Neuropathological staging studies have suggested that tau pathology spreads through the brain in Alzheimer’s disease (AD) and other tauopathies, but this study aimed to reveal more about how neuroanatomical connections, spatial proximity, and regional vulnerability affect this process.
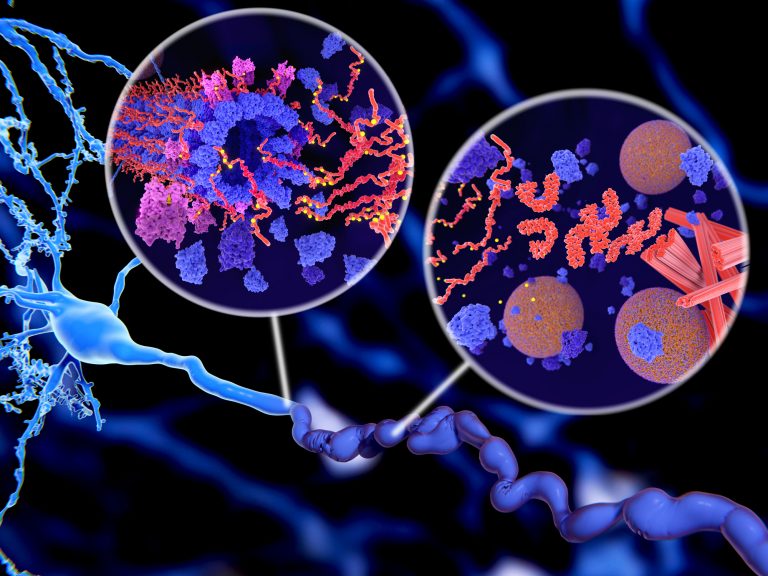
“While the interconnected structure of the brain is essential to its function, these misfolded proteins commandeer that structure to travel through the brain and cause progressive degeneration,” said Michael X. Henderson, PhD, an assistant professor at Van Andel Institute and corresponding author of the study. “By understanding how these proteins travel through the brain and what causes certain neurons to be at risk for damage, we can develop new therapies that can be directed to the right place at the right time to have maximal impact on disease progression.”
It’s estimated that neurodegenerative diseases, including AD and Parkinson’s disease (PD), affect over 60 million people worldwide, and their incidence is expected to soar as the population ages.
The presence of pathological protein inclusions, along with neurological symptoms, are used to distinguish between such conditions. There is overlap in both symptoms and pathologies, especially as the diseases progress. Tau pathology appears prominently in PD, PD dementia, and dementia with Lewy bodies, where it correlates with cognitive decline.
In this study, the researchers started by seeding tau in the brains of non-transgenic mice through intracranial injection. They write: “Tau pathology in this model begins slowly, first affecting the injection site and highly connected regions. As time progresses, more regions are affected.” Previous studies suggest this spatiotemporal pattern of tau pathology reflects spread along neuroanatomical connections.
Next, they quantified pathology over nine months in 134 brain regions. They found that tau pathology moved from region to region along the brain’s neural networks, but that it did not travel to every connected region.
They reported that “One remarkable finding from this analysis was that once pathology seeds a region, it continues in an almost linear fashion over time in most regions suggesting that the process of pathology formation is similar across the brain.” They added that “The lack of a plateau in most regions also suggests that this model is recapitulating the early disease process, before the saturation of pathology and profound neuron death.” The process of pathology formation was reportedly similar across regions, however, the delay between injection and pathology formation varied widely.
To find out why some areas of the brain seemed to resist the proteins’ spread, the team looked at gene expression patterns. They identified some genes that were expressed more in regions that had more tau pathology than expected from protein spread alone.
The researchers also found that spread of the pathology is altered in mice with a mutation in leucine-rich repeat kinase 2. While the spread in these mice is still constrained by anatomical connectivity, it tends to progress in a retrograde direction.
“We used these network models to test our hypothesis that tau spreads both forward and backward along connections between brain regions,” said Eli Cornblath, PhD, an MD/PhD student at University of Pennsylvania and the study’s first author. “After using our models to account for this two-way spreading process, we found several genes that could help inform new molecular targets to clear or prevent these protein aggregates from forming.”













