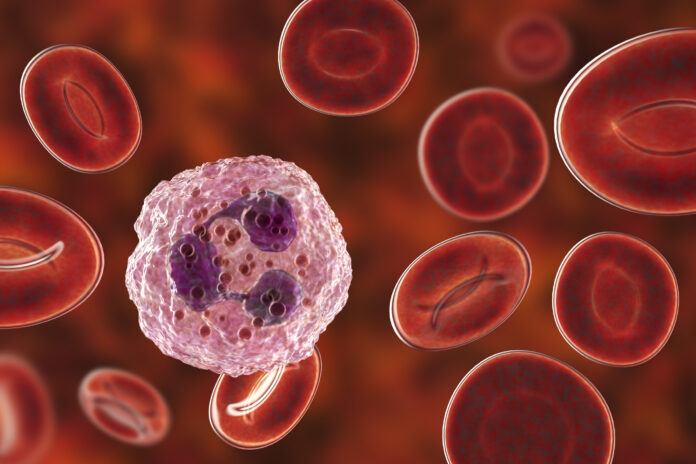
A new study, led by investigators at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine, has demonstrated for the first time the method by which immature neutrophils, a type of white blood cell are controlled by pancreatic cancers to drive both immunosuppression and treatment resistance.
The paper, published in Cancer Discovery, describes a previously unrecognized signaling circuit in pancreatic cancer that instigates immunosuppression and tumor-promoting inflammation in the pancreatic tumor microenvironment, ultimately creating treatment resistance. The central regulator of this treatment resistance is neutrophil-derived tumor necrosis factor (TNF) signaling.
This is the first study to implicate immunosuppressive signaling from immature neutrophils—the earliest sentinels in developing pancreatic cancer—in this process, said Jashodeep Datta, M.D., associate director of Translational Research at the Sylvester Pancreatic Cancer Research Institute, and senior author of the study.
“It suggests neutrophils are a dominant actor in this circuit. This is the first description of how cancer cells talk with neutrophils and how neutrophils are major actors in this immunosuppressive inflammatory drama in the pancreatic tumor microenvironment,” said Datta, the DiMare Family Chair in Immunotherapy at the Miller School.
He said the research is critical to scientists’ knowledge of pancreatic cancer – one of the most treatment-resistant cancers – because it “connects the molecular dots between the high-risk tumor genotypes that exist in pancreatic cancer and the specific molecular and cellular culprits – the immature neutrophils – that are involved in creating immunosuppressive networks in the pancreatic tumor microenvironment.” The research team, Datta said, is “creating a road map to target each element of these molecular dots” to thwart this inflammatory process and overcome therapeutic resistance.
Not only are we creating a roadmap to target each element of these molecular dots, but we are focused on thwarting inflammatory signaling from immature neutrophils, which has never been identified before, in order to overcome therapeutic resistance in pancreatic cancer,”
Nipun Merchant, M.D., the founding director of the Sylvester Pancreatic Cancer Research Institute and a co-author of the paper, said the research “will pave the way to the ultimate goal of clinical studies, so that our findings can be directly translated to improve patient care.”
According to the investigators, their work is the first time a study has implicated immunosuppressive (also called tolerogenic) signaling from immature neutrophils, which are a very important arm of the immune system.
To make the discovery, the Sylvester team collaborated with researchers in different disciplines at the Miller School, including the departments of Microbiology and Immunology, the Diabetes Research Institute, and Public Health Sciences. They also worked with colleagues at other medical schools and cancer centers, including Johns Hopkins, the University of Pennsylvania, and Harvard.
“In order to do super high impact factor translational research, you can’t work in a vacuum,” said the study’s first author Anna Bianchi, a Ph.D. student in the Datta Lab. “Our work is a cross-pollination between the advances we have made at Sylvester and leading expertise nationally and globally. While our team has driven the work, the emphasis is always on team science.”
The researchers used an array of technologies for the research, including single-cell biology, where they used spatial techniques to understand cellular relationships in the pancreatic tumor microenvironment. In addition, the team used high-dimensional sequencing to understand how cancer cells and neutrophils orchestrate this crosstalk. Using these data the researchers then sought to translate the information into the clinic using certain drugs to overcome chemotherapy resistance in cellular and animal models, while also collecting blood samples and tissue specimens made available by patients at Sylvester.
“The whole point is this is extremely clinically actionable data,” Bianchi added.
Now, the focus moves to clinical trials, which will attempt to target the immunosuppressive pathway from numerous angles.
“We’re collaborating with multiple groups across the country to make this happen and are developing a novel nanoengineering platform to target neutrophils without killing them so we can target the tolerogenic [immunosuppressive] signaling mechanisms within neutrophils,” Datta said.













