A small research study carried out in Seoul in South Korea suggests transplanting fecal microbes from cancer patients who respond to immunotherapy could help improve the treatment response in non-responders.
The small study, published in the journal Cell Host & Microbe, showed improved therapy responses in six out of thirteen patients with gastrointestinal cancers who had previously not responded to immune checkpoint inhibitor therapies.
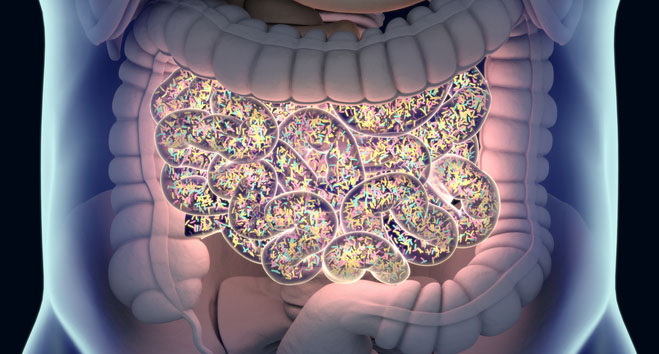
“This research highlights the complex interplay between beneficial and detrimental bacteria within the gut microbiota in determining treatment outcomes,” said co-lead author Hansoo Park, MD, PhD, a researcher at the Gwangju Institute of Science and Technology in South Korea, in a press statement.
“While the connection between gut microbiota and immune response to cancer therapy has been a growing area of interest, our study provides concrete evidence and new avenues for improving treatment outcomes in a broader range of cancers.”
Over the last two decades, the cancer immunotherapy revolution has changed the face of cancer treatment. Some cancers can protect themselves by stimulating immune checkpoints such as PD-1 that dampen the body’s immune response. Immune checkpoint inhibitor drugs can block this defense and help fight cancer and led to James Allison, PhD, and Tasuku Honjo, MD, PhD, winning the Nobel Prize in Physiology or Medicine in 2018.
Although these drugs can be very effective, around half of patients given checkpoint inhibitors do not respond. A number of research groups and biotechs around the world have linked the gut microbiome of patients to poor response to checkpoint inhibitors.
For this study, the researchers recruited four gastric cancer, five esophageal cancer, and four hepatocellular carcinoma patients with metastatic disease who were previously resistant to the PD-1 inhibitor nivolumab.
They extracted fecal microbiota samples from six donor patients with gastric cancer, esophageal cancer, or hepatocellular carcinoma, who had had a complete or partial response to treatment with nivolumab or pembrolizumab for at least six months. These were then transplanted to the gut of the 13 non-responders.
Of the six patients who responded to treatment after their fecal microbiota transplantation (FMT), one had a partial response to treatment and five achieved stable disease.
“One of the most surprising results was from a hepatocellular carcinoma patient who initially showed no response to the first FMT and continued to experience cancer progression. However, after switching the donor for the second FMT, the patient exhibited remarkable tumor shrinkage,” said co-lead author Sook Ryun Park, MD, PhD, a researcher at the Asan Medical Center at the University of Ulsan College of Medicine in Seoul.
“Both donors were long-lasting, good responders to anti-PD-1 inhibitors, but because we did not yet know the causative bacteria responsible for the FMT response, we could not predict whether the treatment would be effective.”
The researchers evaluated the fecal microbiota samples more closely to try and find out which bacteria were changing the therapeutic effects of the checkpoint inhibitors, and which were linked to success of the FMT.
The research is still at an early stage, but the team did identify a new species Prevotella merdae immunoactis that seemed to improve the efficacy of the FMT. They also identified two strains, Lactobacillus salivarius and Bacteroides plebeius, that seemed to increase the likelihood of the FMT failing.
“This study not only demonstrates the broad applicability of FMT in enhancing immunotherapy efficacy, but also opens new paths for targeted microbial interventions in cancer treatment,” concluded the authors.













