French and Swiss researchers have uncovered the genetic and energetic characteristics of leukemic stem cells that are responsible for acute myeloid leukemia (AML) and suggest that blocking a specific iron utilization process of these cells provides an avenue for new therapeutic strategies to fight this disease.
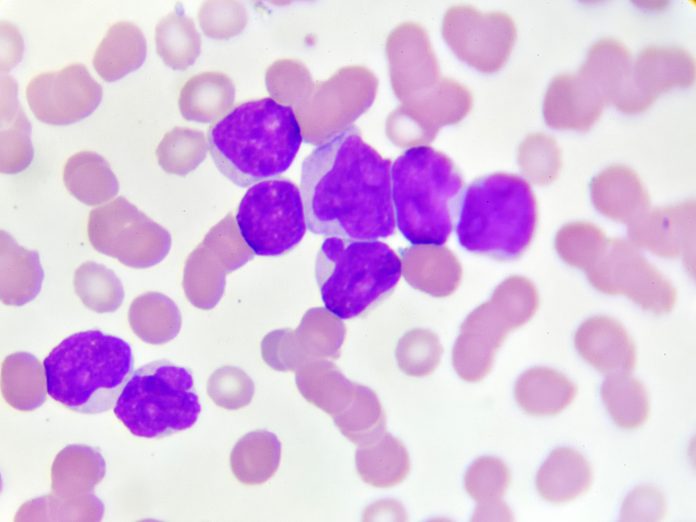
New approaches are desperately needed to treat AML—the most common blood and bone marrow cancer in adults. AML is highly resistant to current treatments. Half of the people under the age of 60 who have the disease die from it, and it is lethal in 85% of those over that age. Researchers surmise the disease is difficult to treat due to quiescent (dormant) leukemic stems cells (LSCs) that evade chemotherapy agents. These cells, which remain intact after first treatments, can become active again spurring redevelopment of AML.
Targeting these stem cells would be an effective method of treating the disease to slow or prevent relapse, but the mechanisms of these cells is not well understood. This new identification of the metabolic characteristics of LSCs by the team from the University of Geneva (UNIGE), University Hospital of Geneva (HUG), and Inserm, published in the journal Science Translational Medicine, provides novel insight into how these cells operate and suggests ways to disrupt them.
Lead researcher for this project was Jérôme Tamburini, PhD, associate professor in the department of medicine and the Centre for Translational Research in onco-hematology (CRTOH) in the UNIGE Faculty of Medicine. He said: “Using advanced bioinformatics techniques and in collaboration with the team of Petros Tsantoulis, MD, PhD, from the department of oncology and precision oncology at the HUG, we first established that these quiescent cells contain a unique genetic signature consisting of 35 genes. When we used this signature in large clinical databases of patients with AML, we were able to show that this signature was strongly linked to the prognosis of the disease.”
Once the team confirmed this link to disease progression, they then sought to find the metabolic differences between dormant and active LSCs. Delving into the chemical reactions within the cells to break down nutrients to provide energy for the cells and autophagy—the process that allows cells to recycle cellular components to provide energy in the absence of external nutrients, they made an important discovery: the dormant LSCs depend on a specific form or autophagy called ferritinophagy, which targets the main iron storage molecules of iron within the cells, ferritin.
“This process is mediated by a protein called NCOA4. It controls the availability of iron in cells. By inhibiting it, either genetically or chemically, we observed that leukemia cells, especially dormant stem cells, are more likely to die, whereas healthy blood stem cells remain intact,” explained first author Inserm researcher Clément Larrue, PhD, a former post-doctoral researcher in the Tamburini lab, now a researcher at the Toulouse Cancer Research Center.
Armed with this knowledge the team then turned to mouse models of AML and confirmed that blocking the protein NCOA4, reduced the growth of tumor cells, reduced their viability, and hindered the self-renewal of LSCs. This suggests that targeting ferritinophagy via this inhibition pathway is a promising therapeutic strategy to fight AML. The compound the team uses to block NCOA4 is currently in preclinical development with the aim of using it in future clinical trials.













