Vienna-based OncoOne is taking aim at developing highly tumor-targeted radioimmunotherapy (RIT) treatments against a range of solid tumors using its proprietary PreTarg-it platform. The two-step process of delivering bispecific antibodies directly to the tumor site shows potential to significantly reduce the side effects associated with treating solid tumors with RIT. Inside Precision Medicine recently took the time to chat with company CEO Randolf Kerschbaumer.
IPM: When was OncoOne founded and what is the focus of the company?
Randolf Kerschbaumer: OncoOne was founded in 2018 and indeed we were framing the company around the target, oxMIF (oxidized macrophage migration inhibitory factor), that had been described several years before—and our team, we have quite some experience in that target. So, we anticipated to generate a panel of antibody modalities in order to target oxMIF for different indications, but with the main focus on oncology.
We find and detect oxMIF in different solid tumors, but we never were able to detect it in healthy tissue. It’s very disease specific and tumor specific. What we also know is that antibodies specifically targeting oxMIF penetrate the tumor and accumulate in the tumor, very efficiently. It was then our consideration how to efficiently bring cytotoxic activity with the antibody into the tumor, and that’s how we then designed the PreTarg-it platform.
Can the PreTarg-it platform also be used for developing diagnostics?
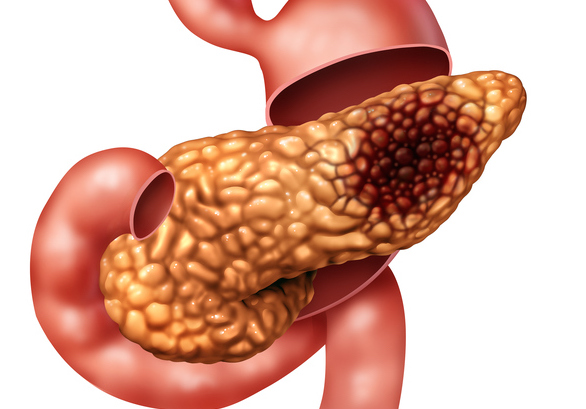
Kerschbaumer: Actually, the PreTarg-it platform is designed to be both therapeutic as well as diagnostic, so it’s a theranostic. If we use a small molecule—the second compound that is applied in the course of a treatment that is labeled with a positron emitter—this can be used for a PET scan, as a diagnostic. We have seen that oxMIF can be detected or occurs very early in the development of solid tumors. For example, oxMIF can be detected in pancreatic cancer very early at stage one. That’s the potential of the diagnostic. But by changing the radionuclide with the second compound, a therapeutic nuclide can be applied, for example, lutetium or actinium, so an alpha emitter or beta emitter, and that has therapeutic potential.
Can you describe why pre-targeting the cancer cells is proving to be an effective method for radioimmunotherapy for treating solid tumors?
Kerschbaumer: When we designed the PreTarg-it platform, we saw that antibodies that are directly labeled with the cytotoxic radionuclide, when they are applied into the body of the patients, they distribute throughout the body. So they’re in the circulation, and also penetrate first into healthy tissue, and it takes a while until the antibody with the directly labeled antibody goes into the tumor and then affects the tumor. It also takes a while until the antibody clears from the circulation, as well as from healthy tissue and this can cause side effects in sensitive tissue, especially in the central nervous system which is quite sensitive to radiation. Our consideration was, if we divide the accumulation in the tumor and clearance from the application of the radionuclide, then we might avoid these negative side effects. By applying the antibody first that is non-labeled, the antibody goes into the tumor and is cleared from the circulation. We can utilize the high specificity of the antibody. in the second step, we give the small molecule, which is a peptide carrying either the cytotoxic nuclide, or the diagnostic nuclide, that goes quite rapidly into the tumor, because it’s a very small peptide. It is also rapidly cleared from the circulation. This way we can avoid a long exposure of healthy tissue to radiation.
How long would a typical treatment cycle last with this kind of therapeutic?
Kerschbaumer: We anticipate that the antibody will take up to a week in order to be accumulated in the tumor and cleared from the circulation. That’s how we design the antibodies. And then the second compound, the radioactive compound, will be applied to the patient. It will be in the circulation for a couple of hours before it concentrates in the tumor, but then it will reside in the tumor for several hours, up to a couple of days—that depends on the half-life of the nuclide that is chosen for the therapy.
OncoOne released encouraging data recently in Molecular Cancer Therapeutics on your lead candidate ON105 that is designed for the treatment of pancreatic cancer. Are you developing other therapeutics for additional cancers?
Kerschbaumer: Yes. PreTarg-it is a platform, and the antibody constructs are very flexible and can be applied to any target of interest. Our first focus is pancreatic cancer simply because we think the big value of the platform is to treat cancers where a rapid readout is required, because the life expectancy of these patients is often very short and you need a fast effect. As we discussed before, the entire treatment cycle is maybe one week, 10 days and in our animal models, we got the effect in one treatment cycle. So the overall platform can be expanded, and we are about to expand it also to other indications. The big value we see is hard-to-treat cancers like ovarian cancer, or head and neck cancer, or gastric cancer.