Researchers have hypothesized how post-viral fatigue syndromes, including Long COVID, become chronic diseases and why patients suffer frequent relapses. In a report published in Cancer, researchers from Otago University, Victoria University of Wellington, and University of Technology Sydney, developed a unifying model to explain how the neurologically-centered symptoms of these diseases are sustained through a brain-body connection.
“This work highlighted that there is a susceptible subset of people who develop such syndromes when exposed to a severe stress, like infection with COVID-19, or the glandular fever virus Epstein Barr, or in some people with vaccination that is interpreted as a severe stress,” says lead author Emeritus Professor Warren Tate, of the University of Otago’s Department of Biochemistry.
Arising most commonly from a viral infection, Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS), can also be caused by other severe stressors such as exposure to agricultural chemicals or surgery. In long COVID, risk factors include being female, older age, obesity, asthma, and poor overall pre-pandemic physical and mental health.
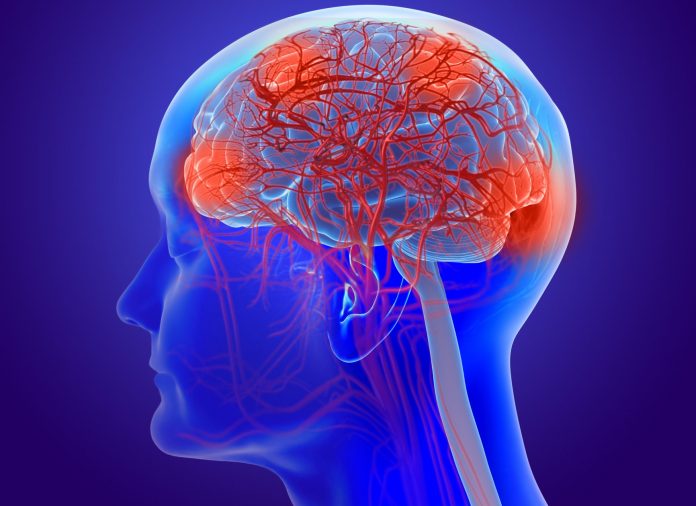
The condition features brain-centered symptoms of neuroinflammation, loss of homeostasis, brain fog, lack of refreshing sleep, and poor response to even small stresses.
Since the 1930s there have been 75 reported outbreaks of probable viral origin that have led to long-term diseases that have the profile of ME/CFS. The current worldwide prevalence of the condition has been reported as between 0.4 and 2.6% among countries meaning it is approximately 10-fold more prevalent than other fatigue illnesses, such as multiple sclerosis.
How these debilitating brain effects develop is poorly understood, and the lack of conclusive biomarkers for a diagnostic laboratory test and the ill-defined pathophysiology have hindered an understanding of the disease.
However, studies have shown ongoing immune dysfunction in ME/CFS patients, both in the blood borne immune cells and in the immune regulator molecules (cytokines) that they export. ME/CFS patients’ immune systems are described as “chronically activated or in overdrive” these authors point out. Cytokine signatures characteristic of the severity of the disease are mainly proinflammatory.
This team suggest that, following an initial viral infection or stressor event, the subsequent systemic pathology moves to the brain via neurovascular pathways or through a dysfunctional blood-brain barrier. This results in chronic neuroinflammation, leading to a sustained illness with chronic relapse recovery cycles.
The model proposes healing does not occur because a signal continuously cycles from the brain to the body, causing the patient to relapse.
The creation of this model is not only important for the “huge research effort ahead”, but also to provide recognition for ME/CFS and Long COVID sufferers.
“These diseases are very closely related, and it is clear the biological basis of Long COVID is unequivocally connected to the original COVID infection – so there should no longer be any debate and doubt about the fact that post viral fatigue syndromes like ME/CFS are biologically based and involve much disturbed physiology,” Tate says.
“Patients need appropriate affirmation of their biological-based illness and help to mitigate the distressing symptoms of these very difficult life-changing syndromes which are difficult for the patients to manage by themselves.
“What should be a transient inflammatory/immune response in the body to clear the infection, develop immunity and manage the physiological stress, becomes chronic, and so the disease persists.”













