Research suggests that a build-up of abnormal microRNAs could be behind the increased risk for Alzheimer’s disease seen in patients who experience traumatic brain injury.
Results from an animal study carried out at the Walter Reed Army Institute for Research in Maryland showed that micro(mi)RNA changes after brain injury led to increased levels of beta-site amyloid cleaving enzyme (BACE1), which generates amyloid beta peptides – a known precursor of Alzheimer’s and other neurodegenerative diseases.
People who have a traumatic brain injury are known to be at significantly increased risk for developing dementia or conditions such as Alzheimer’s after they recover from the initial injury. However, the specific molecular reasons for this neurodegeneration are unclear.
MiRNAs are small pieces of RNA that help to regulate gene expression. As dysregulation of miRNAs have been linked to neurodegenerative conditions and a higher level of cell death after brain injury, Bharani Thangavelu, National Research Council Associate at the Institute, and colleagues decided to investigate links between brain injury and abnormal miRNA build-up.
The team carried out a study in rats with penetrating ballistic-like brain injury and compared brain tissue samples with those taken from control rats. As reported in the journal Frontiers in Neuroscience, build up of more than 800 different miRNAs was recorded, as well as changes in gene expression following injury.
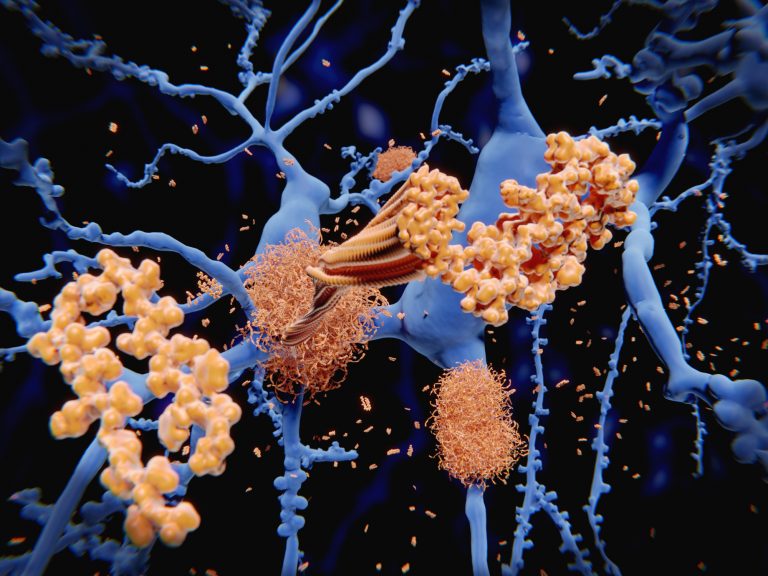
The researchers noted significant differences in miRNA levels in samples taken from rats with brain injury versus those without. The rats with brain injury also had high levels of BACE1 protein. BACE1 breaks down amyloid precursor protein into amyloid beta particles, which are present in patients with Alzheimer’s and some other neurodegenerative diseases. Levels of amyloid beta were noticeably high around 7 days after injury.
“MiRNAs are increasingly recognized as mediators of injury,” noted Angela Boutte, Ph.D., section chief of molecular biology and proteomics at the Institute and senior author of the study.
“It is quite remarkable that BACE1 and amyloid precursor protein are hubs for the miRNA affected by traumatic brain injury. This work infers that there may be underlying common features of traumatic brain injury and Alzheimer’s disease that have not been seen before.”
The team hopes the miRNAs that were dysregulated, as well as BACE1, may serve as useful biomarkers for neurodegenerative disease onset in patients with traumatic brain injury.
Effective treatments for Alzheimer’s disease and other similar conditions remain elusive, with many clinical trial failures over recent years. But the authors believe their findings could help develop more targeted treatments for neurodegeneration triggered by brain injury.
“MiRNAs regulate broad networks of genes. Thus, identifying those which are dysregulated as a consequence of traumatic brain injury offers a means to elucidate molecular mechanisms, or hubs, that underlie neurodegeneration and may serve as viable therapeutic targets,” conclude the authors.











