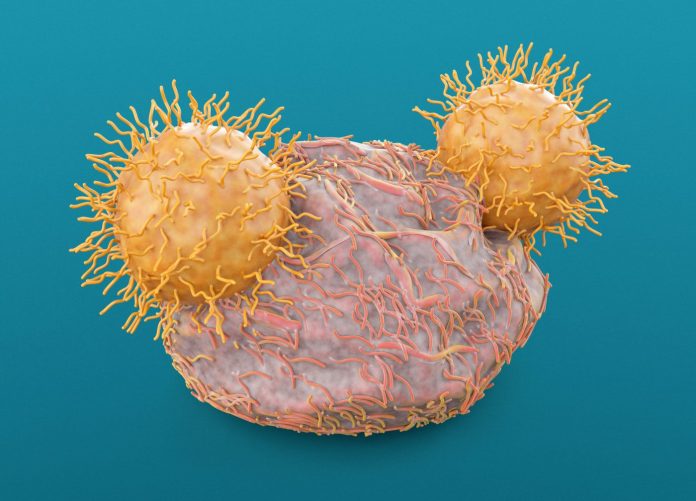
Chimeric antigen receptor (CAR) T cell therapy has exhibited very promising results as a treatment for blood cancers such as leukemia and lymphoma. However, the immunotherapy’s ability to deliver similar results is solid tumors has been hampered by the tumor microenvironment which attacks the CAR T therapy. Now, researchers at Memorial Sloan Kettering Cancer Center (MSKCC) have found that adding a mutated gene could boost CAR T as a treatment for solid tumors. Their research was published in Nature Cancer.
“The CAR T cells are not powerful enough to overcome this inhibition and kill the cancer cells,” says thoracic surgeon Prasad Adusumilli, MD, a CAR T cell researcher at MSKCC. “They go to the tumor site, but then their attack against the cancer peters out.”
The genetic mutation in the c-KIT gene—which has also been found to aid the ability of cancer cells to grow, multiply, and survive—helped the CAR T cells gain strength to fight solid tumors longer than the therapy without the mutated c-KIT gene. The investigators also showed they could regulate the c-KIT effect with a drug “like turning a volume know up or down,” the team wrote. This ability could enable modified CAR T cell therapy effects to allow it to be more safely applied as a treatment.
Adusumilli said the idea to use a cancer mutation to aid CAR T cells came as a result of the understanding that solid tumors continuously reprogram themselves as a defense against treatments. This is often accomplished by cancer cells mutating a single gene which then alters the tumor microenvironment.
“I’ve been thinking of different approaches for making CAR T cells more powerful against solid tumors,” Adusumilli says. “And then the light bulb went off—why can’t we exploit a gene mutation that a cancer cell uses to gain strength for our treatment and give cancer a dose of its own medicine?”
There are a range of mutations that drive cancer growth and spread, which presented a challenge to the MSKCC team in deciding which mutation they should target for study. In the end the team decided to use a mutation that had already been studied extensively, whose effects in cancer were already well understood. Using a mutation that can drive cancer growth was a high-risk proposition “so we thought it best to have a mutation for which effective therapies already exist—that way we can block it if something goes wrong,” Adusumilli says.
The team settled on c-KIT, since mutations in this gene are found in many cancers, and a specific mutation called KITv has undergone the extensive examination they were looking for. A number of tyrosine kinase inhibitors (TKIs) that target KITv have already received regulatory approval. Further, recent research has revealed that addressing solid tumors with CAR T required them to the use the interferon gamma signaling pathway. KITv is known to enhance the interferon gamma signal in CAR T cells.
CAR T cells that are effective for treating blood cancers have incorporated costimulatory signals called CD28 or 41BB, which have been proven to not be strong enough to work against solid tumors. To test KITv, the MSKCC team treated humanized animal models with tumors from mesothelioma, lung cancer, and prostate cancer. The KITv-enhanced CAR T cells showed better anti-tumor effects than either the CD28 or 44BB CAR Ts, with the KITv CAR T cells retaining their ability to self-renew and continue fighting the tumor—without toxicity. CAR T cells that contained both CD28 and KITv were even more effective against the tumors.
With these promising findings, Adusumilli’s team are now applying for grants to conduct a clinical trial for KITv CAR T cells, most likely in mesothelioma. “Translating this approach to the clinic will be challenging, but it also holds great potential,” he says.













