Intestinal cells can change specializations during their lives, driven by the BMP signaling pathway, an important communication mechanism between cells, shows research from an international team of scientists.
The team, headed by the labs of Hans Clevers, PhD, at Hubrecht Institute, and Ye-Guang Chen, PhD, at Tsinghua University, suggest that their work offers new insights into potential targets for the treatment of metabolic diseases. “We knew that BMP signaling plays an important role in the initial specialization of intestinal cells,” stated Joep Beumer, PhD, one of the researchers on the project at the Hubrecht Institute. “What we now discovered is that it is also the driver of changes in the specializations of these cells over their lifetimes.”
The study, reported in the journal Cell Reports, carried out in gut organoids, and in live mice, could also have implications for future research strategies, Clevers suggested. “The study is mainly a fundamental discovery on how intestinal cells differentiate. Our findings do have implications for organoid models, mini-guts grown in vitro: standard protocols would block BMP signaling in these cultures, but we now evidence that activation of BMP signaling is required to represent certain intestinal functionalities in these cultures.”
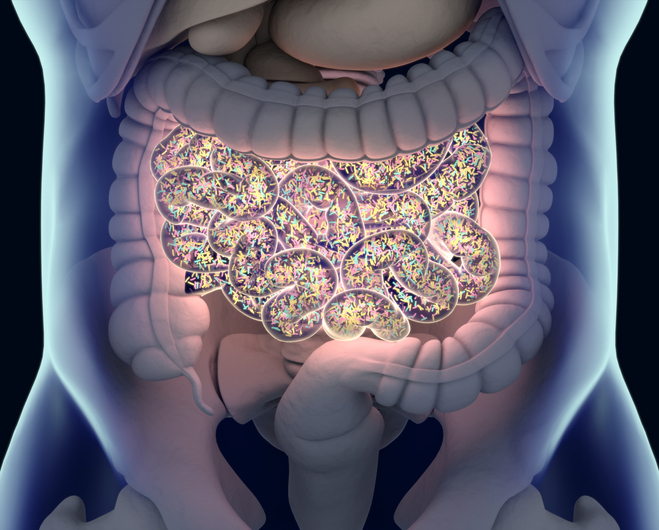
The small intestinal epithelium is the fastest dividing tissue in humans, with an estimated turnover time of about one week, the authors explained. This intestinal wall is made up of different types of cells. Some are, for example, responsible for the uptake of nutrients, while others produce hormones. It was long thought that after their formation, intestinal cells specialize in one function that they continuously perform until they die. However, recent studies show that these cells can change specializations. The newly reported research has now discovered that these changes are driven by the BMP signaling pathway.
Intestinal cells arise from stem cells that lie in indentations (the crypts) of the intestinal wall. These intestinal cells then migrate up the intestinal villi. During their migration, they perform a certain function, for example the absorption of nutrients or the production of hormones. Once they reach the top of the villi, they die. “The function of intestinal cells changes during their migration along the villi,” said Beumer. “They for example produce antimicrobial components in the lower parts of the villi (at the start), while they are involved in absorbing fats later on in their journey.”
This gradual change in the function of the cells is called zonation. At the same time, the BMP signaling pathway is not very active in the crypts and in the lower parts of the villi, while it becomes more and more active higher up in the villi.
Clevers further explained, “Previous bodies of research suggested that major functional intestinal cell types (nutrient—absorbing enterocytes, mucus-producing goblet cells) appeared to specialize in different functions along the crypt-villus axis. This is the axis cells travel along after their birth in the crypt bottom, a journey ended by cell death at the villus tips. We investigated what signaling pathways drives these changes along the crypt-villus axis.”
The BMP signaling pathway is one of many signaling pathways in the body. Such pathways form lines of communications between cells: with the production of a protein by one cell, it gives a signal to the next cell, which in turn produces proteins. Eventually, this whole cascade of protein production triggers certain processes—for example processes that are important during embryonic development.
The scientists at the Clevers lab used intestinal organoids for their research. These are tiny 3D structures that can be grown in the lab and that mimic the function of the gut. In these miniature guts, the researchers were able to mimic conditions of low or high BMP signaling, similar to the altering environment along the intestinal villi. Using single cell RNA sequencing, a technique that makes it possible to see which genes are active and which ones are not, they made a surprising discovery.
Hubrecht Institute researcher, Jens Puschhof, PhD, noted, “When BMP was active in the organoids, the cells in these miniature guts were identical to the cells located in the top of the villi, while inactivation of BMP made the cells in the organoids resemble the cells located in the lower parts of the villi. In other words, zonation turned out to be dependent on the BMP signaling pathway.” As the team commented in their published paper, “Using human intestinal organoids, we show that BMP signaling controls the expression of zonated genes in enterocytes,” the investigators noted. “We find that goblet cells display similar zonation involving antimicrobial genes.”
Clevers summed up the findings. “Our study explains how cell types that are mature when exiting the crypts (already absorbing certain nutrients, or producing antimicrobial proteins) can alter their function over their lifetime. A BMP morphogen gradient, low in the crypt/villus bottom and increasing towards the villus tip, drives these functional changes in intestinal lineages. An example: enterocytes appear to specialize in lipid uptake (under the control of BMP signaling) in the villus tip, while absorbing nutrients and producing antimicrobials in the bottom villus (low BMP).”
The researchers also confirmed their results from experiments in the organoids in mouse models. Colleagues from the group of Chen used a mouse model in which BMP signaling could be turned off in the gut. In mice with an inactive gut BMP signaling pathway, intestinal cells no longer changed specialization during their migration from the crypts to the villi. “Using an inducible Bmpr1a knockout mouse model, we confirm that BMP controls these zonated genes in vivo,” the team further wrote. “That confirmed our conclusion: BMP signaling is the driver behind zonation of intestinal cells,” added Beumer.
The findings may have important implications for the use of organoids for research, the investigators suggest. “Normally, researchers inhibit BMP signaling in organoids,” said Hubrecht Institute co-author Fjodor Yousef Yengej, PhD. “Although this proved beneficial for growth, not all functions of the gut are represented in these cultures.” Activation of BMP signaling may be required for research into certain topics, such as fat absorption. In addition to providing these new fundamental insights into the functions of intestinal cells during their lives, the study may ultimately contribute to the development of new treatments for metabolic diseases.
“Our findings imply that local manipulation of BMP signal strength may be used to reset the enterocyte ‘‘rheostat’’ of carbohydrate versus lipid uptake and to control the antimicrobial response through goblet cells,” the scientists pointed out.
“In certain metabolic diseases, there is an accumulation of fat in parts of the body such as the liver, or an imbalance in gut hormones,” Beumer noted. “We now know that active BMP signaling stimulates fat absorption, so if we can inhibit signaling in these patients, we can also influence fat absorption.” BMP inhibitors targeting the gut are yet to be developed, but would have broad beneficial effects on metabolism.
The authors further concluded, “Our observations may have therapeutic implications for lipid uptake-related diseases … Our findings emphasize the potential of intestine-specific BMP inhibition for diseases related to excess lipid uptake from food.” Clever pointed to the potential goals of continued work. “We are interested in the mechanisms of BMP-regulated changes in intestinal lineages,” he said. “We would like to know which BMP ligands and receptors are involved. Finally, we are investigating the metabolic consequences of BMP inhibition. We predict that lipid uptake would be reduced, but also other changes occur in intestinal lineages that could profoundly impact nutrient uptake/hormone secretion from the gut, with potential applications for metabolic diseases.”





![Comprehensive Genomic Profiling at Diagnosis Extends Survival in Patients with Advanced Cancer Harmonizing NGS standards is expected to provide a strong evidence base for decisions on coverage of clinical genomic testing and treatment for cancer. [iStock / zmeel]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/507-218x150.jpeg)







