Calibr, the drug discovery and development division of Scripps Research, reports positive Phase I results for its next generation switchable CAR-T cell therapy platform in patients with B cell cancers.
In a presentation today at the CAR-TCR Summit in Boston, the researchers announced that six of nine patients treated with the new type of cell therapy had a complete response.
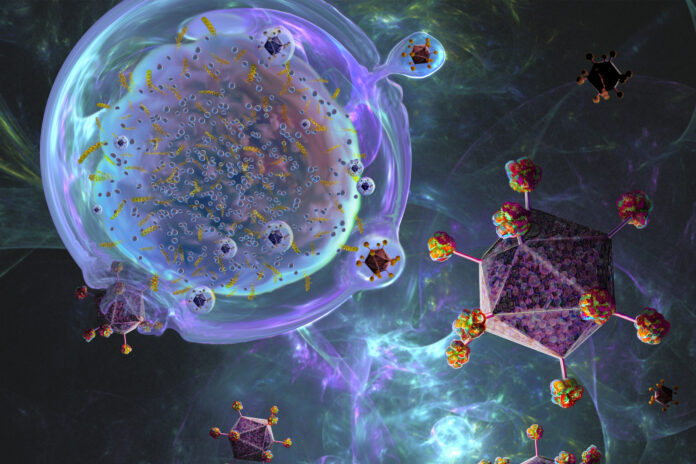
CAR T-cell therapy, where a patients T cells are extracted and modified to fight their cancer before being re-injected, have revolutionized cancer therapeutics with many unexpectedly positive responses in late-stage blood cancer patients. However, they do come with high side effect risks.
CAR T-cell therapies are prone to overactivation and they can be very dangerous, causing potentially catastrophic immune reactions in some people. While there are treatments to combat these adverse effects, there is now a new generation of CAR T-cell therapies in development that aim to solve this problem with the addition of “on” or “off” switches. These switches can be used to either switch on the therapeutic effect or switch it off if it becomes overactivated, for example, often using a small molecule drug as an activator or stop signal.
Calibr has a focus on further development of research and possible new drugs and therapies developed by Scripps Research, previously known as The Scripps Research Institute. In addition to several other academic groups and organizations and some companies, they have developed a switchable CAR T-cell therapy platform in collaboration with big pharma company AbbVie.
The current report focuses on the first nine patients recruited into an ongoing Phase I trial of Calibr’s first switchable CAR-T cell product (CLBR001 + SWI019) for treatment of B cell malignancies. Calibr’s CAR-T cells are initially inactive and are activated only when dosed with the tumor-specific antibody “switch” (in this case the anti-CD19 SWI019 switch).
All the participants had already been extensively treated with a median of five cancer therapies. Treatment with the new cell therapy resulted in an overall response rate of 78% and a complete response rate of 67%, often with just one therapy dose.
Immune effector cell associated-neurotoxicity syndrome (ICANS) and cytokine release syndrome (CRS) were less frequent, less severe and shorter in duration (2–3 days vs 5–17 days) than with first generation CAR-T cell therapies, which the research team attribute to the switchable nature of the new therapy.
“These results underscore the potential of Calibr’s switchable CAR-T cell platform to act like a ‘software’ and ‘hardware’ approach, where the biological response of the CLBR001 cell ‘hardware’ can be programmed using the switch dose as the ‘software’,” said Travis Young, vice president of biologics at Calibr.
“This is our first step toward demonstrating the potential of this universal platform to be programmed toward any target, including those for solid tumors.”













