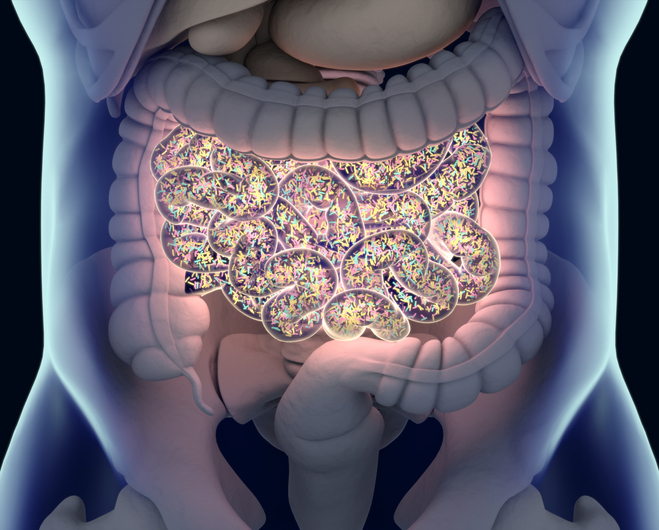
Two separate studies published today in Cell Host & Microbe have found that myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is associated with reduced levels of microbes known to produce the fatty acid butyrate in the gastrointestinal microbiome. The researchers say this finding could partly explain how the immune system becomes disrupted in people suffering from ME/CFS.
“It’s important to note that this research shows correlation, not causation, between these microbiome changes and ME/CFS,” said Julia Oh, an associate professor at the Jackson Laboratory and senior author of one of the two papers. “But these findings are the prelude to many other mechanistic experiments that we hope to do to understand more about ME/CFS and its underlying causes.”
Brent Williams assistant professor at Columbia University and senior author of the second paper noted “This research demonstrates that there are robust bacterial signatures of gut dysbiosis in individuals with ME/CFS. It helps to expand on this growing field of research by pinpointing the structural and functional disturbances in the microbiome in a chronic disease that affects the quality of life of millions of people.”
ME/CFS is a chronic, complex, and systemic disease associated with neurological, immunological, autonomic, and energy metabolism dysfunctions, whose causes have remained elusive. The disease has been difficult to study as it tends to be heterogenous and people with ME/CFS present was a range of different symptoms. However, the has recently emerged as a potential contributor to ME/CFS.
In Oh’s study, the team used shotgun metagenomics to compare microbiome samples from 74 people with both short-term ME/CFS, defined as those diagnosed in the previous four years, and 75 long-term ME/CFS patients—those with symptoms for more than 10 years. The study also included 79 age- and sex-matched healthy controls.
Analysis fond that patients with short-term disease had a number of changes to the diversity of their microbiomes, notably a depletion of microbes known to be butyrate producers. Butyrate helps protecting the integrity of the gut barrier and is also plays an important role in modulating the immune system.
By comparison, long-term ME/CFS patients had gut microbiomes that had reestablished and were more similar to the healthy controls. However, those participants had accumulated a number of changes in the metabolites in their blood plasma, including many of those related to the immune system. They also had differences in levels of certain types of immune cells compared with the healthy controls.
Oh added that future studies will focus on further subdividing patients by the features of their disease, including those with conditions frequently associated with ME/CFS such as irritable bowel syndrome and neuroinflammatory disorders. “This will help us pinpoint specific microbial and metabolomic factors that are associated with this disease,” she said.
The Columbia research led by Williams also used shotgun metagenomic sequencing to look at the microbiomes of 106 people with ME/CFS and 91 healthy controls that were matched for age, sex, geography, and socioeconomic status. This study recruited patients from five different sites across the US, to help control for microbiome differences that may be present in different geographic regions. The study also looked at levels of microbial species in the stool.
This study found significant relationships between the severity of fatigue symptoms and levels of specific species of gut bacteria, in particular a specific butyrate-producing bacterium called Faecalibacterium prausnitzii. It also revealed a higher overall load of bacteria in the stool and disturbances in the interactions among bacterial species in patients with ME/CFS.
“While these findings don’t unequivocally demonstrate causative relationships between disturbances in the microbiome and symptoms, these microbiome-symptom relationships present potentially actionable, manipulatable targets for future therapeutic trials,” Williams noted. “These trials could perhaps focus on dietary, probiotic, prebiotic, or synbiotic interventions and could provide direct evidence that gut bacteria influence chronic symptom presentation.”













