Depending on which research report is referenced, there are anywhere from a couple hundred to more than 600 bispecific antibodies (bsAbs) in preclinical and clinical development by pharma and biotech companies around the world.
Nine of the 12 bsAbs that have received approval globally target cancer. But after the first marketing approval of a bispecific antibody—catumaxomab in 2009, targeting malignant ascites—the well went dry. It was five years before another bsAb was granted approval—blinatumomab from Amgen for the treatment of relapsed or refractory precursor B-cell acute lymphoblastic leukemia (ALL)—and another three years after that until Roche’s hemophilia drug emicizumab reached that milestone.
Another four years then elapsed until Janssen’s amivantamab came to market for the treatment of non-small cell lung cancer in May 2021. At last, the floodgates opened for this promising class of drugs, with six bsAbs approved in 2022, two more so far in 2023, and pipelines brimming with dozens of bsAbs currently in Phase II and Phase III clinical trials.
But why did it take so long for the development of bsAbs, a therapeutic class with so much potential to change the landscape of cancer treatment, to come to fruition?

professor
Department of Hematopoietic Biology and Malignancy, Division of Cancer Medicine
MD Anderson Cancer Center
According to Jeffrey Molldrem, MD, a professor in the Department of Hematopoietic Biology and Malignancy, Division of Cancer Medicine at MD Anderson Cancer Center, “I think people in the [bsAbs] field had been trying for a long time but had met with some challenges. We did too,” he says. “Some of those were because the antibody bound to HLA mostly and not the peptide.”
But there were other challenges as well.
“The field itself had to come up with better ways to purify these antibodies, which was a trick because most of the bispecifics are very difficult to purify,” Molldrem adds. “We’ve also had to enhance stability and then improve the pK. Those improvements have been made.”
The next generation of cancer therapy
Among the many avenues taken for cancer treatment in the past 20 years, the promise of unleashing or aiding the immune system to attack cancer has been the most promising. Immuno-oncology today is applied both as active therapies such as cancer vaccines and CAR T-cell therapies that target cancer cells using the immune system, and in passive forms such as checkpoint inhibitors that help enhance the body’s own immune response to quell cancer development. Yet while monoclonal antibodies, checkpoint inhibitors, and cytokines have improved cancer care either as monotherapies or in combination with other treatments, only some patients respond to these therapies, and even those who do respond will eventually see their cancer return or metastasize.
CAR T-cell therapy for certain hematologic malignancies broke stunning new ground in immunotherapy with the approval of Kymriah in 2017, which boosted five-year survival rates from 10% to nearly 50%. But serious adverse events—notably cytokine release syndrome (CRS)—affect roughly 30% of patients, and many eventually also experience a relapse of disease.
What oncologists have been looking for are treatments that can largely avoid the development of drug resistance to provide high response rates with minimal side effects. These are the characteristics of bispecific antibodies that have so many in the field excited and have spurred pharma and biotech companies to fill their pipelines with this class of candidates.
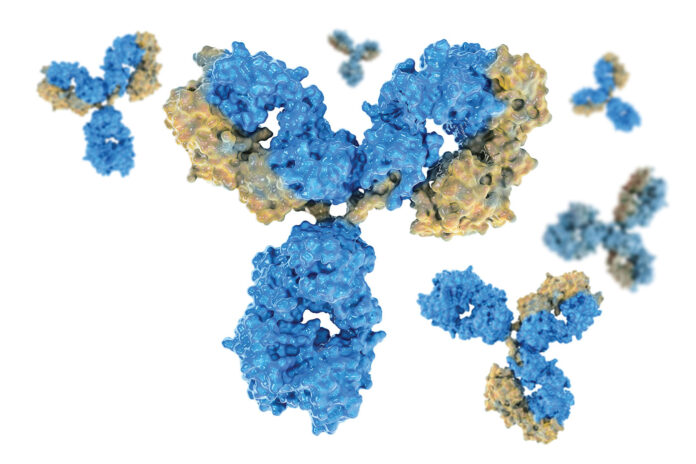
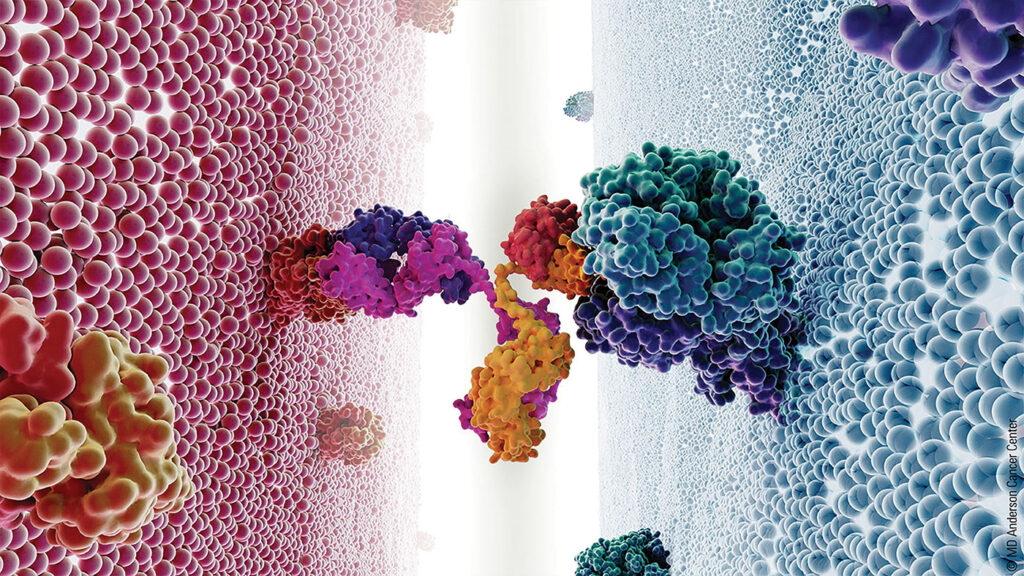
One advantage over monoclonal antibodies is that instead of two arms of the antibody having the same specificity, on the engineered bsAbs each of the two arms are directed at different targets. For instance, in the case of two recently approved drugs for relapsed or refractory diffuse large B-cell lymphoma, Epkinly from Abbvie and Columvi from Roche, one arm targets the CD20 antigen on B cells, while the other arm targets CD3 on T cells. By addressing two targets with one antibody, bsAbs amp up their ability to fight cancer cells. By targeting antigens only found on the blood cells themselves, they greatly reduce the occurrence of CRS.
In addition to those targeting blood cancers, there are also two approved bsAbs for the treatment of solid tumors (amivantamab approved in May 2021 targeting EGFR and cMet in NSCLC, and cadonilimab, approved in China for cervical cancer and targeting PD-1 and CTLA-4). But progress in this area has been more challenging. That said, bsAbs for solid tumor treatment are making inroads addressing targets currently treated with checkpoint inhibitors or checkpoint blockade, as well as ones that target tumor-associated antigens (TAAs). The main targets for solid tumor bsAbs are the usual suspects: HER2/HER3, EGFR, CTLA4, and PD-1/PD-L1.
Some of the difficulty in generating meaningful response in solid tumors is related to the relatively short plasma half-life of bsAbs. In hematologic malignancies, the bispecific is introduced directly to the source of the cancer, the patient’s blood. For solid tumors, it takes extra time for the antibodies to reach the tumor site via the circulation. Limited biodistribution, tumor microenvironment (TME)-mediated resistance, development of anti-drug antibodies, and on-target resistance are all hurdles that needed to be cleared. But recent advances in understanding tumor biology and the TME are allowing drug developers to engineer different forms of bsAbs, with clinical trials targeting solid tumors in Phase II and later showing the same promise as those for treating blood cancers.
Response rates and adverse events
All of the six bsAbs for hematologic malignancies are approved for very late stage or metastatic disease, often after four or more lines of treatment have already failed. But even in this setting, with patients who are weakened and often have severely compromised immune systems, bsAbs have shined.

associate director
Multiple Myeloma Clinical Research Program
Dana-Farber Cancer Institute
“Right now, the single-agent response rates for teclistamab (a bsAb targeting BCMA/CD3 for relapsed and refractory multiple myeloma) is about two-thirds, so well over 60% of patients respond,” notes Omar Nadeem, MD, associate director of the Multiple Myeloma Clinical Research Program at Dana Farber Cancer Institute. “For most other agents being studied in this space, if you had a response rate somewhere around 30% that was considered a successful, promising agent until these immune therapies came out. These therapies have shifted our expectations.”
Murali Janakiram, MD, a hematologist-oncologist at City of Hope with clinical expertise in multiple myeloma, notes that the less severe side effects experienced by patients treated with a bsAb is currently a key factor, since they are often a treatment of last resort, given to patients who are very weak and may not qualify for CAR T therapy.

hematologist-oncologist
City of Hope
“Bispecific antibodies recruit innate cells to fight the myeloma, while CAR T cells multiply after administration, and that is why cytokine release syndrome is much more common in that form of treatment,” Janakiram says.
Rates of CRS for bsAbs treating hematologic cancers are around 36%, compared with CAR T, which has a rate of about 90%, he notes. But the rates of Grade 3 or Grade 4 CRS, which can be life-threatening, are also low with CAR T, at around 3% to 5% of cases.
Differences in delivery can also help mitigate the risk of CRS. CAR T cells are given in a one-time infusion, while bsAbs are given as a priming dose followed by regular fixed duration administration via an injection or IV infusion. “The rates and the intensity of CRS for biospecifics is significantly less, partially because you can titrate them in,” says Tahi Ahmadi, CSO of Genmab. “You don’t have that opportunity with CARs, you just give them and then they do whatever they do.”
Likewise, the neurological adverse event ICANS (immune effector cell-associated neurotoxicity syndrome), which is also common in CAR T, occurs in just 1% to 2% of patients receiving bsAbs.
“With ICANS, the CAR T cells can easily go into the CNS, while a bispecific antibody structure requires that the CD3 is anchored to the myeloma cell and the antibody itself does not penetrate the blood-brain barrier,” Jankiram adds.
The most common adverse event associated with bsAbs are infections, Nadeem says. “It’s a big issue with bispecifics, they really suppress the immune system and if you start adding other drugs it further suppresses the immune system, so we need to be careful how we dose it.”
Since so many of the bsAbs are so new, more work is needed to determine appropriate dosing levels. For now, Nadeem notes that while he is hesitant to endorse dose scheduling that hasn’t been fully validated, based on the large number of patients he has treated with bsAbs he says patients continue to respond even with less frequent, intermittent dosing.
“We’ve been encouraging a lot of the community providers to not feel the pressure to keep people on this weekly schedule,” Nadeem says. “Because even if you give it to them a couple of times a month, they tend to maintain their response.”
Moving toward first-line treatment
Given the high response rates to bsAbs in heavily pretreated populations, pharma companies are now moving these therapies up the line in clinical trials to treat people much earlier in disease progression, with either bsAbs as a monotherapy or in combination, to test its utility as a first-line treatment.

CSO, Genmab
“That’s our ambition at Genmab,” Ahmadi states when asked if bsAbs will become frontline treatments in the future. But for now, one model he sees playing out is a dual approach in some instances, where chemotherapy has been an effective treatment in certain cancers.
“We can do chemotherapy in those who are fit,” he says. “We are also looking at patients who are elderly and may not necessarily be candidates for chemotherapy because of their comorbidities, but their immune system should still be functional because they haven’t already received all these other therapies that have a negative impact on the immune system.
“Then we are looking at it as single agent, or in combination, and asking the question: ‘Can we get the same result without patients ever seeing chemotherapy?’”
Nadeem, Janakiram, and Molldrem all agree that bsAbs will eventually move to frontline therapies either in combination or as single agents, noting that some clinical trials are already underway to test these therapies in early treatment settings.
“We think immunotherapy makes a lot more sense earlier,” Nadeem says. “If you really want to utilize the immune system, then the best way to do that is when the disease is less heavily pretreated.” In fact, researchers at Dana Farber are currently enrolling patients in a Phase II clinical trial of high-risk smoldering myeloma, for which there are no current treatments, to determine whether the disease can be treated early with good results.
With promising results and a pathway to frontline treatment, might bsAbs supplant CAR T therapy for the treatment of hematologic malignancies?
“I’m pretty certain that is going to be the future, but we all have our biases,” Ahmadi notes. “I don’t think CAR T ever got close to giving the return on investment. In five years, I just don’t see how an individualized, process-challenged approach can compete with something that is off the shelf.”
Janakiram sees it differently. “I still think CAR T has its unique advantages. The fact that it is a one-and-done therapy appeals to so many people,” he points out. “I think, over time, the manufacturing time for copies will come down and the side effect profile will improve. I see CAR T and bispecific antibodies as two different things and they are going to complement, rather than supplant, each other.”
BsAbs in the community setting
While CAR T immunotherapy will likely be here for some time, in its current form it requires specialized skills, takes weeks to harvest the cells then engineer them for reinfusion, and delivery is limited to a small handful of leading cancer centers. What excites many about the coming wave of bsAbs is their potential to be given to patients in the community setting, as they are an off-the-shelf therapy.
“At the point of care, it is much harder to do any kind of cell therapy,” Molldrem notes. But “with bispecifics, it’s off the shelf and you can deliver it just like any other antibody.”
As Nadeem sees it, much of the danger of adverse events from bsAbs comes during the priming dose, and that leaves the possibility of performing initial dosing in the community setting “an open topic” among clinicians. Dana Farber is currently managing the initial dosing, and once it is clear a patient is tolerating the treatment, they are moved back to a community site. Nadeem also believes this will change in the coming years as methods will be developed to pretreat patients prior to the priming dose, and dosing levels will become more precise.
“I think we’ll figure out a way to do this safely as an outpatient [procedure], and more people will get comfortable with it over time,” Nadeem concludes.
Chris Anderson, a Maine native, has been a B2B editor for more than 25 years. He was the founding editor of Security Systems News and Drug Discovery News, and led the print launch and expanded coverage as editor in chief of Clinical OMICs, now named Inside Precision Medicine.













