Every virus has its preferred niche — a particular host or demographic it is more inclined to infect and a particular set of strategies and tactics it uses to achieve this. A virus develops a niche over millions of years, all the while adapting and mutating in response to host immune defenses. The longer a virus has to get to know a particular host species, the more attuned it becomes. It learns the nuances of the immune system in question, and critically, how to circumvent them; slowly, it focuses its blows on the chinks in the armor, slashes at the Achilles’ heel. But this doesn’t happen in isolation. As the virus adapts, so too does the host immune system it attacks. The two go hand-in-hand.
Human history cannot be separated from this intricate dance with viruses. The COVID-19 pandemic — just like the Spanish flu pandemic of 1918, the polio epidemics of the 1940s and 1950s, and the ongoing HIV/AIDS crisis — makes this crystal clear. With advancements in modern medicine and public health, we have the possibility to shift the tide in our favor. Antiviral drugs and vaccines play an especially important role in this process.
If before our immune system was fighting with a wooden club, we now have the means to supply it with a shield and sword. Even so, the effectiveness of vaccines and antivirals fluctuates according to the virus at hand. This means that, although there are general guidelines and preventative measures that can be applied to pandemic preparedness across the board, each virus will have its own specific dynamics that require us to make adjustments at a more granular level. Studying previous pandemics can help us understand how differences in viral niches and viral strategies may influence what kind of response is needed, particularly in regards to the role of vaccines and antiviral drugs.

Nature knows best: vaccines
When discussing successful vaccination campaigns, it is impossible not to make mention of poliomyelitis. Polio, as it’s more commonly known, is a disease caused by a small, single-stranded RNA virus. For the most part, people infected with the poliovirus are none the wiser: 70% of poliovirus infections are asymptomatic and a remaining 20-25% are only mildly symptomatic.
But at the tail end of distribution, there are those who go on to develop fatal complications. Around 1% of those infected end up suffering from paralytic polio, the most severe form of the disease1. This is characterized by excruciating pain that radiates through the back and lower limbs. The hallmark of paralytic polio, and the reason it is so infamous, is eventual paralysis of limbs. This happens when the virus travels from the bloodstream into the spinal cord, infecting and damaging motor neurons. Paralysis can extend to the diaphragm, leaving certain patients unable to breath on their own. Without access to a respirator, this quickly leads to death. Some individuals may recover, but if motor function doesn’t return to normal within the span of a year, it is generally accepted that paralysis will be lifelong.
Despite the fact that only a small subset of those with polio suffer serious disease, the ease and extent to which it spreads causes huge issues—a small subset of a very large number quickly becomes quite large itself. At the height of the global polio epidemics, more than half a million people were left paralyzed or dead by the virus each year2.
The development of vaccines in the 1950s and the 1960s, however, has allowed us to eradicate poliovirus from endemicity in all but two countries, Afghanistan and Pakistan.
The first vaccine for polio, developed in the 1950s by Jonas Salk, helped protect against severe disease and paralysis, but did not prevent transmission. It works by exposing our immune system to an inactivated, or killed, version of the poliovirus. Because the inactivated polio vaccine (IPV) uses killed virus, there is no chance of viral mutation causing a reversion to the original pathogenic form. Although not perfect, the vaccine quickly helped curb the worst of the polio endemics. A second polio vaccine was developed in the 1960s by Albert Sabin. Unlike its predecessor, it has the distinct advantage of also preventing transmission. The oral polio vaccine (OPV) uses an attenuated, or weakened, version of the poliovirus. This elicits a stronger, more robust immune response. The fact it can prevent transmission truly kickstarted poliovirus eradication, lending solidity to what may have initially seemed a pipe dream.
Like poliovirus, many SARS-CoV-2 infections are asymptomatic. Even more cause only mild disease. But for a few, infection will lead to serious, life-threatening disease. Unlike poliovirus, SARS-CoV-2 continues to circulate globally at nearly the same rate despite the development of vaccines.
Why? Because poliovirus and SARS-CoV-2 inhabit very different niches and make use of different strategies. In a sense, the two viruses work on opposite sides of the street.
Poliovirus, by and large, relies on what we call “the fountain of youth,” i.e., the fact that new human beings are born all the time. Infants and young children have a naive immune system, making them more susceptible to infection. Poliovirus exploits this fact, and it does so extremely well: the overwhelming majority of polio cases are seen in children under the age of five. Crucially, polio is a “one-and-done” kind of virus. Once someone has been infected, they essentially develop lifelong immunity. This is why complications are only seen in the immune-naive population — all others who were already infected and had no issues are no longer at risk.
This leads us to a fundamental lesson in vaccinology. If in nature you become immune by infection, then we can generally make an effective vaccine; if in nature you do not become immune by infection, then it is generally very difficult to make an effective vaccine.
This is why the vaccines we have for SARS-CoV-2 only protect against disease, not against infection and transmission. Unlike poliovirus, SARS-CoV-2 has developed extremely precise strategies to evade and suppress our immune system, allowing it to infect a large spectrum of people3. This includes adults with fully developed immune systems. As such, it thrives in a much more immune-experienced niche than poliovirus. The complex immunoevasive abilities of SARS-CoV-2 mean it can infect, reinfect, and then reinfect again.
This is complicated by a further tactic: antigenic variation. Essentially, mutations to the genetic material of the virus that cause its surface proteins, or antigens, to undergo structural changes. These changes render the virus unrecognizable to our immune system, despite having been exposed to a previous version of the virus. Even within the same variant family the changes can be large enough to dodge our built up immunity. The result? Annual or bi-annual waves of infection spearheaded by new variants that our immune system cannot defend against. This is evidenced by Omicron BA.5 and BA.2.75, which are causing new spikes in cases just as the wave caused by the original Omicron variant begins to recede.
The difficulty of containing SARS-CoV-2 via vaccination should come as no surprise. Influenza virus has been with us for a lot longer, and still it infects upwards of 1 billion people every year, causing roughly 300,000 to 650,000 deaths4. The reason is similar: influenza mutates at an extremely high rate, creating new sub-clades all the time. These sub-clades can then go on to reinfect us in a cyclical fashion, known as flu season. We have vaccines for the flu, but again they only stop disease, not transmission. In fact, the H1N1 subtype of the influenza A virus, which is to blame for most infections, is a descendant of the virus that caused the 1918 Spanish flu pandemic. So even a hundred years later, we continue to feel its effects.
Vaccination campaigns were indispensable to controlling and resolving the polio epidemics of the 1940s and 1950s. They have continued to be central to eradication efforts ever since. A vaccine that helps prevent transmission is still far away in the case of SARS-CoV-2, if it ever arrives. This difference between poliovirus and SARS-CoV-2 drives home a key point: we cannot rely solely on vaccines to contain or eradicate SARS-CoV-2. Future pandemics may be similar in this regard — within the influenza family, too, there are many strains that we know little about and that may not permit us the luxury of eradication simply through vaccination.
Polio aside, there is another epidemic we can learn from, one where there are no vaccines to speak of.
Lessons from HIV/AIDS: prophylactic drugs
On June 5, 1981 the United States Centers for Disease Control and Prevention (CDC) published a report describing five cases of a rare lung infection, pneumocystis carinii pneumonia, in the Los Angeles area5,7. All five cases were in young gay men who were in good health before the onset of symptoms. Along with the pneumonia, all of the men also had other unusual infections. Their immune systems were clearly not working as they should be. At the time of publication, two of the men had already passed away. The remaining three men passed away shortly after. A year later, in September of 1982, the CDC gave the disease an official name: acquired immunodeficiency syndrome (AIDS). It took until 1984 for the cause of AIDS to be discovered, a retrovirus initially labeled HTLV-III, now known as human immunodeficiency virus (HIV).

More than 40 years have passed since that initial report and HIV/AIDS continues to be a public health issue in many parts of the world. There is no cure for the disease and, as mentioned, we do not have a vaccine. I suspect we may never develop a vaccine like the ones we have for polio. This has to do with the particularly crafty nature of the virus.
Like influenza and SARS-CoV-2, and unlike poliovirus, HIV infection does not lead to lasting immunity. On the contrary, HIV infection means persistent, life-long infection; our immune system just can’t get rid of the virus, allowing it to replicate and circulate indefinitely. Once HIV has entered the body, it quickly begins infecting immune cells — the very cells that we usually rely on to fight infection. Its primary targets are T helper cells. These have a number of important immune functions, including: the activation of small signaling proteins, called cytokines, that help initiate the inflammatory response and call other immune cells into action; the production of killer T cells which destroy cancer cells, cells infected by pathogens, and cells damaged through other means; and finally, they also maximize the antibacterial activity of phagocytes, which ingest foreign invaders. HIV infection of T helper cells destroys them, leaving them functionally useless. With time, the number of T helper cells drop below a critical level, causing a complete attrition of cell-mediated immunity. This leaves HIV-positive individuals at an extremely high risk of opportunistic infections and cancers.
As with SARS-CoV-2, HIV is a master of evading our immune system. The immune cells it infects act as a disguise, providing the virus with a reservoir to replicate undisturbed and unseen. As long as there is a single latent reservoir, the infection can bounce back to full force without much trouble. Added to this is the fact it replicates at break-neck speed, brute forcing its way past our immune system, which simply can’t keep up. And not only is the replication cycle fast, it also churns out massive amounts of mutations. This leaves us with many different strains, all circulating at the same time. For now, this combination of factors has bested all attempts at vaccine development.

Regardless, we have made tremendous progress.
The biggest contribution, aside from the fervent activism that set things in motion, has come from investment in and development of pre-exposure prophylaxis (or PrEP) medicine. PrEP medication helps prevent HIV infection and can be taken by HIV-negative individuals at high-risk of exposure. We also have effective treatment options for HIV-positive patients: antiretroviral therapy. These suppress viral load to undetectable levels, eliminating the risk of the virus being transmitted to an HIV-negative partner. Together, the two drug therapies make for a powerful combination — one helps prevent those who don’t have the virus from contracting it, the other helps prevent those who do have the virus from passing it on.
At the personal level, these drugs mean that HIV infection can now be managed, allowing HIV-positive individuals to live long, healthy lives. At the population level, these same drugs act as a containment mechanism, serving to curb the spread of the virus. The blueprint is clear: learn as much about a given pathogen as we possibly can and then use this newfound knowledge to develop prophylactic drugs that help render it de facto irrelevant. This is what has been working for HIV/AIDS, it is what will work for SARS-CoV-2, and it is also what will work for future pandemics that cannot be solved solely through vaccination. Of course, this won’t happen overnight; it requires persistent effort, resources, and funding. It also requires international collaboration and, perhaps most importantly, a certain amount of political will.
References
1. Mehndiratta, M. M., Mehndiratta, P., & Pande, R. (2014, October). Poliomy elitis: Historical facts, epidemiology, and current challenges in eradication. The Neurohospitalist. Retrieved July 2022.
2. Canadian International Immunization Initiative (CIII) & Canadian Public Health
Association (CPHA). (2004, December). The end of polio is within our grasp… but
major challenges remain to reach goal by 2005. Retrieved July 2022.
3. Haseltine, W. A. (2021, August 12). How Sars-CoV-2 Evades And Suppresses The Immune System (Part 1). Forbes. Retrieved July 2022.
4. World Health Organization. (2019, March 11). WHO launches new global influenza strategy. Retrieved July 2022.
5. A Timeline of HIV and AIDS. HIV.gov. (2022, April 29). Retrieved July 2022.
6. Ståhl, P.L., et al., Visualization and analysis of gene expression in tissue sections by spatial transcriptomics. Science, 2016. 353(6294): p. 78-82.
7. Centers for Disease Control and Prevention. (n.d.). Pneumocystis pneumonia — Los Angeles 1981. Centers for Disease Control and Prevention. Retrieved July 2022.
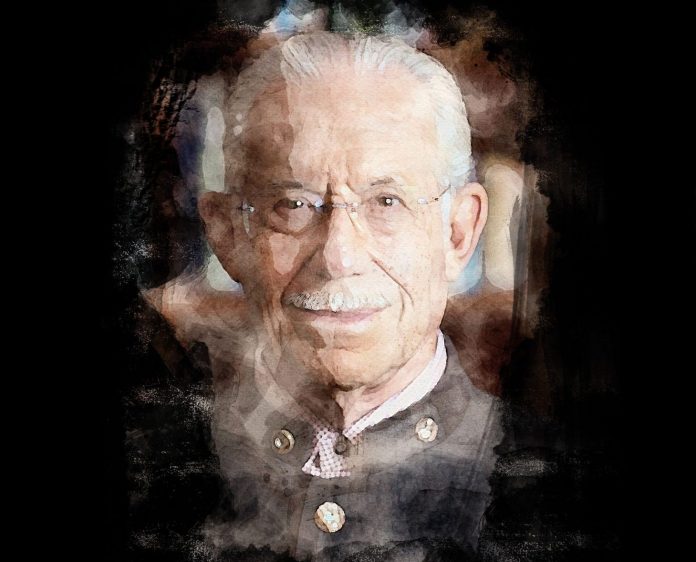
William R. Haseltine, PhD, is chair and president of the think tank ACCESS Health
International, a former Harvard Medical School and School of Public Health professor and founder of the university’s cancer and HIV/AIDS research departments. He is also the founder of more than a dozen biotechnology companies, including Human Genome Sciences.













