Scientists at Baylor College of Medicine have demonstrated that in animal models of breast cancer and prostate cancer, eliminating the gene SRC-3 specifically in a type of immune cell called regulatory T cells (Tregs) triggered a lifelong anticancer response that eradicated the tumor without the typical side effects observed with other therapies.
The research also showed that transferring Tregs without SRC-3 to animals carrying breast cancer tumors resulted in long-term elimination of the tumor without negative side effects.
“Other published treatments seem to reduce tumor burden or eliminate the cancer for some time, but in most cases, it returns,” said Sang Jun Han, PhD, associate professor of molecular and cellular biology in the Center for Reproductive Medicine at Baylor, and is also is a member of Baylor’s Dan L. Duncan Comprehensive Cancer Center. “Our findings in animal models are the first to show that Tregs lacking SRC-3 eradicate established cancer tumors and appear to confer long-lasting protection against recurrence.” Han is first author of the team’s published paper, which is titled “Steroid receptor coactivator 3 is a key modulator of regulatory T cell–mediated tumor evasion.” Commenting on their collective findings, the team concluded, “Therefore, treatment with SRC-3-deleted Tregs could represent an efficient future target for eliminating tumor growth and recurrence without the autoimmune side effects that typically accompany immune checkpoint modulators.”
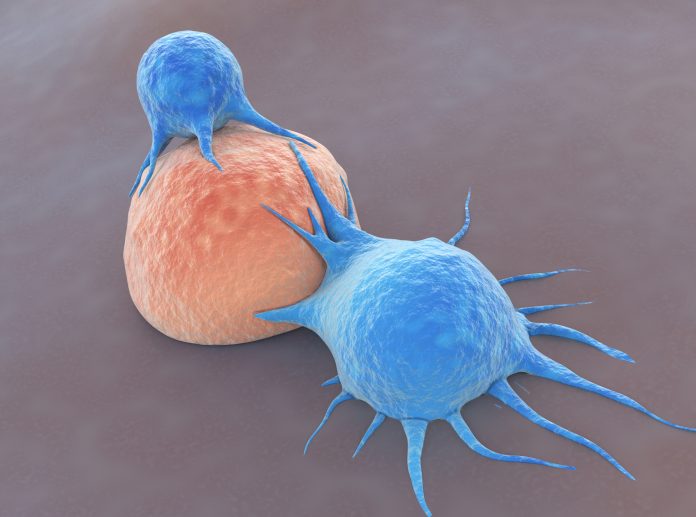
Tregs play an essential role in restraining immune responses to maintain immune homeostasis and prevent autoimmune disease, and are of great interest from an anticancer therapeutic perspective, the authors explained. “Tregs play a critical role in cancer progression by generating an immune-suppressive microenvironment and thus have been a major focus for immune checkpoint inhibitor therapeutic development.”
For their newly reported work, the team focused on SRC-3, which had previously been characterized as a potential oncogene that drives somatic cell cancer progression. Corresponding author Bert W. O’Malley, MD, chancellor and professor of molecular and cellular biology at Baylor, explained further, “More than 30 years ago, my lab discovered a protein we called steroid receptor coactivator (SRC) that is required for the effective regulation of gene activity. “Since then, we have discovered that a family of SRCs (SRC-1, SRC-2, and SR-3), regulates the activity of a variety of cellular functions.”
Over the years, the O’Malley lab and colleagues have been particularly interested in SRC-3 and its role in cancer. SRC-3 is not only highly expressed in all human cancers and plays a role in cancer growth, but it is also strongly expressed in Tregs that regulate the immune response to cancer. It had also been suspected that SRC-3 plays a role in regulating Treg function. “In addition to cancers, we found previously that SRC-3 has a critical role in immune cell function,” the team wrote. “For example, SRC-3 is the most highly expressed transcriptional coactivator in Tregs. SRC-3 is highly expressed in both mouse and human Tregs, and inhibition with an SRC-3 small molecular inhibitor (SI-2) inhibits the immune suppressive function of Tregs,” the investigators further stated.
Intrigued by the abundance of SRC-3 in Tregs and suspecting that it might play a role in controlling cancer progression, O’Malley and his colleagues investigated the effect of eliminating the gene SRC-3 in Tregs on breast cancer growth.
The team generated knockout (KO) mice lacking the SRC-3 gene only in Tregs (SRC-3 KO animals) and then compared breast cancer progression in these mice with the progression in mice that had the SRC-3 gene.
“We were surprised by the results,” O’Malley said. “Breast tumors were eradicated in the SRC-3 knock-outs. A subsequent injection of additional cancer cells in these mice did not give rise to new tumors, showing that there was no need to generate additional SRC-3 knock-outs to sustain tumor resistance. Importantly, transferring these cells to animals carrying pre-established breast tumors also resulted in cancer eradication. We obtained similar results with prostate cancer.”
The authors summarised, “Using genetically engineered Treg-cell-specific SRC-3 KO mice, we show that disruption of Treg SRC-3 expression leads to a complete lifetime eradication of tumors in aggressive syngeneic breast and prostate cancer models.” The results showed that only one injection of the SRC-3-KO cells (adoptive cell transfer; ACT) was needed to achieve a potent antitumor effect. “Importantly, a single adoptive transfer of SRC-3 KO Tregs into wild-type E0771 tumor-bearing mice can completely abolish preestablished breast tumors by generating potent antitumor immunity with a durable effect that prevents tumor reoccurrence,” the team continued.
The investigators in addition discovered that Tregs lacking SRC-3 mediated long-lasting tumor eradication by effectively modifying the environment surrounding the tumor into one that favored its elimination. Using a variety of laboratory techniques, O’Malley and his colleagues showed that the modified Tregs proliferated extensively and preferentially infiltrated breast tumors where they released compounds that generated an antitumor immune response. These compounds facilitated the entrance of immune cells—T cells and natural killer cells—that directly attacked the tumor. The modified Tregs also blocked other immune cells that attempted to stop the anti-tumor response.
“We are very excited about the results; altogether they warrant continuing our investigations to translate the findings into a novel, more effective, and longer-lasting cancer therapy,” said Han. The authors further stressed that their SRC-3 KO Tregs conferred long-lasting protection against cancer recurrence in mice without any apparent systemic autoimmune effects. “In conclusion, we demonstrate that SRC-3 KO Tregs show strong potential as a therapeutic approach for cancer therapy,” they wrote. “SRC-3 KO Treg-based ACT therapy also avoids many of the known limitations seen for other immune-therapeutics, such as membrane immune checkpoint inhibitors, and is effective in breast/prostate mouse tumors where checkpoint inhibitor drugs are less effective.”
O’Malley is principal scientist and director at CoRegen, which is working with Baylor to commercialize the discoveries, and to which all the underlying patents and intellectual property have been licensed.













