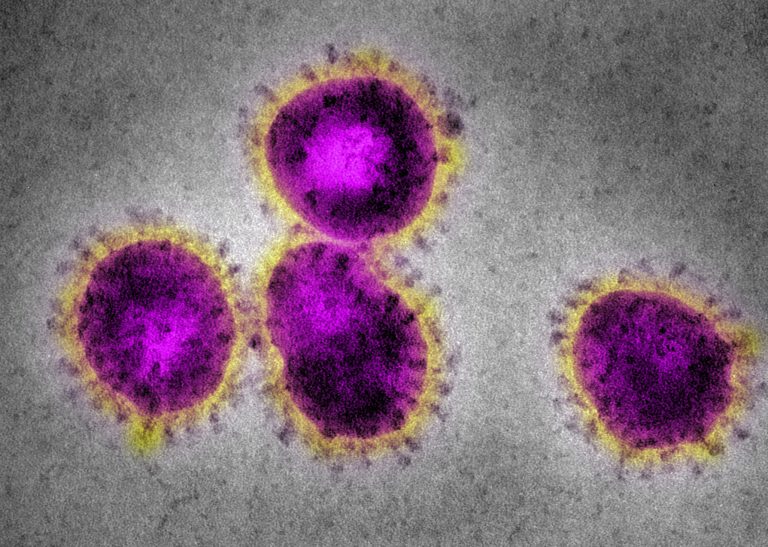
Endpoint Health—a new targeted therapeutics company that uses artificial intelligence—has announced its launch, with personalized treatments to help patients suffering from acute respiratory distress syndrome (ARDS) caused by COVID-19.
The Palo Alto, Calif.-based company is already working with 40 top hospitals in the U.S. and abroad to bring personalized therapies to critically ill patients, including those with sepsis, Endpoint announced July 13.
Endpoint claims to be the first targeted therapeutics company focused on integrated solutions for critical illnesses, combining novel and on-market therapeutics, companion diagnostics and artificial intelligence (AI) into an integrated platform designed to improve outcomes in critically ill patients.
Endpoint’s platform analyzes molecular and digital patient data to find distinct patient subgroups that can then be targeted for specific treatments. The company’s models identify late-stage and on-market therapies—often created for other indications— that Endpoint can develop into targeted therapies, providing the required tests and software to guide their use, the company said. Endpoint’s vision is to empower clinicians with an array of approved therapeutic solutions that can be targeted to each unique patient to improve clinical outcomes.
“One of the biggest ongoing challenges for critical care physicians is treating life-threatening illnesses like sepsis and ARDS,” said Hector Wong, M.D., director of critical care medicine at Cincinnati Children’s Hospital. “These aren’t single diseases, they’re heterogeneous syndromes, and we can see this in clinical practice—some patients respond to a specific therapy, while others with similar clinical presentation don’t.”
“We need to target therapies to the right patient at the right time to gain real improvement,” Wong said. “We’ve seen this approach transform oncology over the last few decades, and I’m excited by the potential for Endpoint’s approach to do the same in critical care.”
Working with Endpoint’s solution, Todd Rice, M.D., director of the medical intensive care unit at Vanderbilt University Medical Center in Nashville, approved of the product, saying it approached solving patient problems the way clinicians do; by untangling their complex nature and personalizing all of the patient’s care. “Critically ill patients require multiple therapies that may range from routine care such as fluids, to novel therapies,” he said. “At the end of the day, if your goal is to improve the outcome of a patient, you have to care about targeting both routine and novel therapies.”
According to Jason Springs, co-founder and CEO of Endpoint Health, critical illnesses make up half of U.S. hospital mortality and over $100 billion of annual U.S. healthcare spend. “Sepsis alone is associated with as many global deaths as cancer each year, and yet patients with these life-threatening illnesses still have few treatment options,” he said.
“The COVID-19 pandemic, which placed unprecedented numbers of patients in the ICU, has drawn the world’s attention to the desperate need for advances in this field,” Springs said. “We need a new approach to how we understand these illnesses, and how we develop and deliver treatments.”
Endpoint was the recipient of $12 million in debt and equity financing from top-tier investors, including Mayfield, Y Combinator, AME Cloud Ventures, and Wireframe Ventures. The company is led by an experienced executive team including the co-founders of GeneWEAVE, an infection detection and therapy guidance company acquired by Roche for $425 million in 2015, Endpoint said.













