Scientists in the Netherlands, U.K., and U.S. report on study results suggesting that a common strain of Escherichia coli gut bacteria could be contributing directly to bowel cancer by releasing a toxin, colibactin, that causes mutations in cells lining the gastrointestinal tract. The studies showed that cells in cultured human mini-guts — human intestinal organoids — developed a unique signature of DNA mutations following months’ of exposure to the pks+ E. coli strain. The same mutations were also subsequently found in the DNA of patients with colon cancer. The study results imply that the mutations were directly induced by the genotoxic E. coli strain and ‘bad bacteria’, the researchers stated, and offer up the first direct link between microbes that live naturally in our bodies and genetic alterations that drive cancer development.
The research was spearheaded by a team headed by scientists at the Hubrecht Institute (KNAW) and Princess Máxima Center in Utrecht, the Netherlands, with £20 million in Cancer Research UK Grand Challenge award funding. “Things like tobacco or UV light are known to cause specific patterns of DNA damage, and these fingerprints can tell us a lot about past exposures that may have caused cancer to start, commented Hans Clevers, PhD, Grand Challenge co-investigator at the Hubrecht Institute. “But this is the first time we’ve seen such a distinctive pattern of DNA damage in bowel cancer, which has been caused by a bacterium that lives in our gut.”
The researchers further suggest that a test for detecting this specific pattern of E. coli-related DNA damage to gut lining cells could be used alongside current bowel cancer screening tests to help identify people at higher risk of colon cancer. It’s also possible that other toxins produced by gut bacteria might have similar effects, the team noted, and researchers are looking at whether this mechanism of DNA damage is more widespread. Clevers and colleagues report on their studies in Nature, in a paper titled, “Mutational signature in colorectal cancer causes by genotoxic pks+ E. coli.”
Bowel cancer represents the second most common cause of cancer death in the U.K., where there are around 42,000 new bowel cancer cases every year. Understanding what the disease triggers are could help doctors to detect colon cancer at its earliest stages, when treatment is most likely to be successful, and could also lead to new approaches to preventing cancer development.
This potential has led scientists to investigate the role that the microbiome may play in the development of bowel cancer. “The intestinal microbiome has long been suggested to be involved in colorectal cancer (CRC) tumorigenesis,” the authors commented. “Various bacterial species are reportedly enriched in stool and biopsies of CRC patients, including genotoxic strains of Escherichia coli (E.coli). These pks+ strains of E. coli produce the toxin colibactin, and have been shown to induce DNA damage in cell lines. The bacteria are found in about 20% of healthy people, 40% of people with inflammatory bowel disease, and about 60% of people with familial adenomatous polyposis and colorectal cancer.
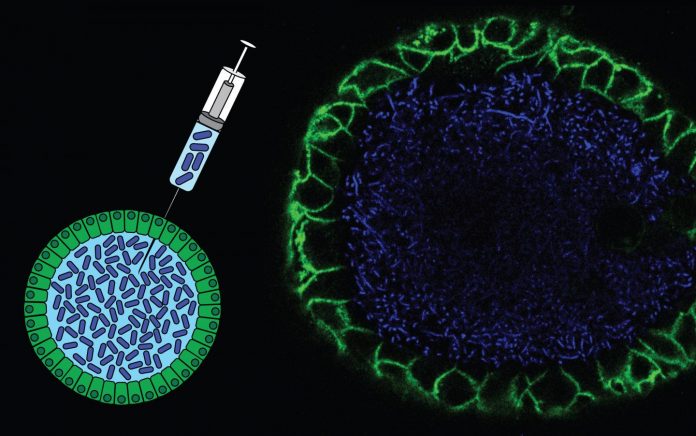
The Clevers team at the Hubrecht Institute focused on these colibactin-producing E. coli strains. Because colibactin can cause DNA damage in cells grown in the lab, they reasoned that the toxin might be doing the same to cells lining the gut. A team of three PhD students from the laboratories of Clevers, and of Ruben van Boxtel, PhD, at the Princess Máxima Center for pediatric oncology, set out to identify the damaging effects of colibactin on human DNA, using the miniature lab-grown human intestine organoids, which represent a model system that had been developed in the group of Hans Clevers.
The team developed a method by which they exposed the healthy human intestinal organoids to the genotoxic E. coli bacteria. After five months of bacterial exposure, the investigators then sequenced the DNA of the human cells to identify the numbers and types of mutations. They found that the genotoxic bacteria-exposed organoids harbored about double the amount of DNA damage, in comparison when compared with organoids exposed to E. coli that didn’t produce the colibactin.
The researchers also discovered that the DNA damage caused by colibactin followed two very specific patterns, which were unique to toxin exposure. Processes that cause DNA damage may result in specific mutation patterns, or fingerprints/signatures, and telltale signatures have already been identified for various cancer-causing agents, including tobacco, smoke, and UV light. The presence of these signatures in tumor DNA can be used to inform about past exposures, which may underlie disease initiation. “These signatures can have great value in determining causes of cancer and may even direct treatment strategies”, explained van Boxtel. “We can identify such mutational footprints in several forms of cancer, also in pediatric cancer. This time we wondered if the genotoxic bacteria also leave their unique distinguishing mark in the DNA.”
Their results showed that genotoxic E. coli bacteria caused two co-occurring mutational patterns in the organoid cell DNA. One signature was characterized by the change of an adenine (A) base to any other of the four bases in DNA code, and the other was the loss of a single A in long stretches of As. In both cases, another A base was present on the opposite strand of the DNA double helix, three to four bases away from the mutated site. “I remember the excitement when the first signatures appeared on the computer screen” said co-author Axel Rosendahl Huber, “we had hoped for some indication of a signature that we could follow up on in other experiments, but the patterns were more striking than any signature we had analyzed before.”

To determine whether the DNA damage caused by the bacterium played a role in bowel cancer, the researchers analysed the DNA sequences of more than 5,500 tumor samples from the U.K. and Netherlands, with the help of Henry Wood, PhD, and Philip Quirke, PhD, from the University of Leeds. First, they looked for the two colibactin DNA damage fingerprints in over 3600 Dutch samples of various cancer types, and found that they were present in multiple tumor types, but primarily in bowel cancers. “This analysis revealed a strong enrichment of the two pks signatures in CRC-derived metastases when compared to all other cancer types,” they wrote.
The researchers then refined their investigation to focus on bowel cancer tumors specifically, and analyzed over 2,000 bowel cancer samples from the U.K., collected as part of the 100 000 Genomes Project run by Genomics England. Among these samples, the colibactin fingerprints were present in 4–5% of patients. This suggested that colibactin-producing E. coli may contribute to 1 in 20 bowel cancer cases in the U.K. “More than 5% of colorectal cancer had high levels of the footprint, while we only saw it in less than 0.1% of all other cancers,” noted co-author Jens Puschhof.
“Imagine studying a gut bacterium’s footprint for months in a dish, and then finding back the same footprint in the DNA of patients.” Only a few other cancers that are known to be exposed to the bacteria, such as cancers in the oral cavity and the bladder, also had the same fingerprint. “The small number of pks signature-positive urogenital and head-and-neck cancer cases suggests that pks+ bacteria act beyond the colon,” the scientists stated. “It is known that E. coli can infect these organs, and we are keen to explore if its genotoxicity may act in other organs beyond the colon. The signature we defined experimentally helps us with this,” Puschhof added.
Further studies will be needed to shed light on just how much of a role the toxin could play in these cases, and what other components of the microbiome may be involved in the early stages of bowel cancer. “This study implies that detection and removal of pks+ E. coli, as well as re-evaluation of probiotic strains harboring the pks island, could decrease the risk of cancer in a large group of individuals,” the investigators noted. “There are probiotics currently on the market that contain genotoxic strains of E. coli,” Clevers pointed out. “Some of these probiotics are also used in clinical trials as we speak … These E. coli strains should be critically re-evaluated in the lab. Though they may provide relief for some bodily discomfort in the short term, these probiotics could lead to cancer decades after the treatment”.
And further down the line, the researchers suggest, looking for DNA damage fingerprints like the ones associated with colibactin in the cells of the gut lining could be used to identify those who are at a greater risk of developing the disease. Philip Quirke, PhD, Grand Challenge co-investigator at the University of Leeds, stated, “Our goal is to understand the causes of bowel cancer, so discovering the role of colibactin represents an important step. As a Grand Challenge team, we are now looking at other bacteria and their toxins associated with bowel cancer, and we hope to identify more DNA damage fingerprints to paint a better picture of risk factors. We will then need to work out how we can reduce the presence of high-risk bacteria in the gut. But this is all in the future, so for now people should continue to eat a healthy diet and participate in bowel cancer screening.”
Nicola Smith, senior health information manager at Cancer Research UK, added, “The more doctors understand about how bowel cancer develops, the better they will be at detecting it and helping people reduce their risk.”













