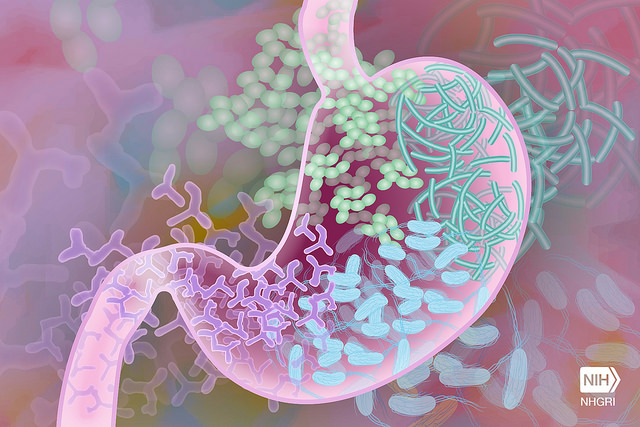
Specific intestinal microbiota signatures correlate with high-grade adverse events and response to combined CTLA-4 and PD-1 blockade treatment, according to a new study from researchers at The University of Texas MD Anderson Cancer Center. The researchers also identified a potential new strategy to treat toxicity, while maintaining response to combined immune checkpoint blockade—either IL-1R inhibition or manipulation of the gut microbiota.
The study was published this in Nature Medicine.
“This study further highlights the importance of the gut microbiome in both response as well as in toxicity in patients being treated with combined immune checkpoint blockade,” said senior author Jennifer Wargo, M.D., professor of Genomic Medicine and Surgical Oncology. “We’re committed to understanding and addressing the significant immune-related side effects that tend to accompany this combination therapy, so that patients don’t have to compromise quality of life for effective cancer treatment.”
The global checkpoint inhibitor market is estimated to be about $15 billion and expected to double within the next couple of years, as more cancer patients get treatment after the COVID-19 pandemic wanes.
Dual immune checkpoint therapy has contributed to progress in overall survival for many cancer types, including advanced melanoma. Combining CTLA-4 and PD-1 inhibitors produces high responses, yet is often accompanied by immune-related adverse events, such as colitis, an inflammatory bowel disease that can cause additional complications. The field currently lacks strong biomarkers to understand which patients are most likely to respond to combined checkpoint inhibitors and which are most likely to develop severe toxicity to the treatment.
This study found a significantly higher abundance of Bacteroides intestinalis in the gut microbiota of patients with advanced melanoma who experienced toxicity from combined immunotherapy. In both patients and preclinical models, a high abundance of B. intestinalis in the gut microbiota was affiliated with increased mucosal IL-1β and associated inflammation. Inhibiting IL-1R with a drug approved to treat rheumatoid arthritis reduced intestinal inflammation without blunting the efficacy in pre-clinical models.
Another bacterium, Parabacteroides distansonis, was associated with response to treatment in both the patient cohort and preclinical models. Gut microbiome diversity wasn’t significantly different between responders and non-responders, contrary to previous research focusing on single-agent immune checkpoint blockade targeting PD-1.
The patient cohort was comprised of 77 adults who received combined CTLA-4 and PD-1 blockade treatment for advanced melanoma at MD Anderson. The majority had stage IV disease (84%) and had not received any previous systemic therapy (74%). Nearly all patients had an adverse event of any grade (93.5%) and about half (49%) experienced grade 3 or higher adverse events in response to treatment.
The research team also studied genomic and immune predictors of response to combined immune checkpoint blockade and identified some associations between immune cell profiles in the blood and toxicity to treatment. Patients who experienced grade 3 or higher adverse events had a more diverse T cell repertoire and a more naïve T cell phenotype in the systemic circulation.
Whole-exome sequencing of 26 pre-treatment cutaneous melanoma tumor samples revealed higher tumor mutational burden (TMB) in responders, compared to non-responders. Non-responders had a higher level of copy number loss, primarily affecting chromosomes 5, 10 and 15. These findings further support previous studies that suggest TMB is associated with response and copy number loss is associated with resistance. Baseline tumor biopsies also revealed a higher density of CD8+ T cells in responders, compared to non-responders.
These results also support previously identified immune and genomic biomarkers for response to treatment with a single immune checkpoint blockade.
“We’re getting closer to understanding which patients are most likely to benefit from checkpoint inhibitors and to identifying strategies to mitigate toxicity,” Wargo said. “We’re grateful to the patients who have participated in our ongoing research; they continue to motivate and inspire us as we undertake additional studies to build upon the insights from this research.”













