New research led by an investigator at Indiana University may a building block for helping to stem the obesity epidemic via targeted treatments versus today’s methods of healthier eating and exercise. The research shows that a stomach-specific protein plays a critical role in the progression of obesity, and could potentially lead to the development of therapeutics that would help individuals struggling with achieving and maintaining weight loss.
The study, “Gastrokine-1, an anti-amyloidogenic protein secreted by the stomach, regulates diet-induced obesity,” was published in the journal Scientific Reports and led by David Boone, Ph.D., associate professor of microbiology and immunology at Indiana University (IU) School of Medicine, and an adjunct professor in the department of biology at the University of Notre Dame.
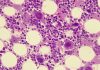
“Obesity and its sequelae have a major impact on human health,” wrote the researchers. “The stomach contributes to obesity in ways that extend beyond its role in digestion, including through effects on the microbiome. Gastrokine-1 (GKN1) is an anti-amyloidogenic protein abundantly and specifically secreted into the stomach lumen. We examined whether GKN1 plays a role in the development of obesity and regulation of the gut microbiome.”
GKN1 is a stomach protein highly expressed in normal gastric tissue and plays a major role in maintaining gastric mucosal integrity. The researchers showed that curbing GKN1 produced significant differences in weight and levels of body fat in comparison to when the protein was expressed.
“While diet and exercise are critical to maintaining a healthy weight, some individuals struggle with weight loss—even in cases of bariatric surgery, maintaining weight loss can be a challenge,” explained Boone. “These results are an example of how a better understanding of the gut microbiome and the physiological aspects of obesity—how our bodies regulate metabolism and accumulate body fat—could help inform new therapies.”
The researchers conducted a microbiome analysis of mouse models with and without the GKN1 protein expressed. They observed models without GKN1 weighed less and had lower levels of total body fat and higher percentages of lean mass. When put on a high-fat diet (HFD), models without GKN1 showed resistance to weight gain, increased body fat, and hepatic inflammation.
“Gkn1−/− mice were resistant to diet-induced obesity and hepatic steatosis (HFD fat mass (g) = 10.4 ± 3.0 (WT) versus 2.9 ± 2.3 (Gkn1−/−) p < 0.005; HFD liver mass (g) = 1.3 ± 0.11 (WT) versus 1.1 ± 0.07 (Gkn1−/−) p < 0.05). Gkn1−/− mice also exhibited increased expression of the lipid-regulating hormone ANGPTL4 in the small bowel. The microbiome of Gkn1−/− mice exhibited reduced populations of microbes implicated in obesity, namely Firmicutes of the class Erysipelotrichia. Altered metabolism consistent with use of fat as an energy source was evident in Gkn1−/−mice during the sleep period,” wrote the researchers.
They did not find any evidence of adverse effects such as cancer, diabetes, loss of appetite, malabsorption, or inflammation. The loss of GKN1 expression is associated with gastric cancer. However, they did not find any evidence of gastric cancer in GKN1−/− mice. “Although we did not observe spontaneous gastric cancers in GKN1−/− mice we cannot rule out the possibility that loss of GKN1 predisposes to gastric cancer in the context of other additional inducers such as inflammation or infection.
Further studies are needed to determine the efficacy of blocking GKN1 to prevent obesity, but this study is a step in potentially creating new therapeutics that could reduce the burden on health care systems and help improve quality of life for patients.