When people think of what causes cancer, they probably think of smoking, too much sun, maybe even diet. Various carcinogens do drive genetic mutations that set off cancers. In some cases, though, someone’s genes at birth—the ones that make up a person’s germline genome—can cause cancer. According to Prasanth Reddy, senior vice president and enterprise oncology head of Labcorp’s oncology unit, about 5–10% of cancers are due to inherited risks.
In the past, scientists diagnosed hereditary cancers from family histories, but today’s oncologists can make use of a range of options, from cancer-related gene panels to complete genome sequencing. As Yuri Fesko, medical director of oncology medical affairs at Quest Diagnostics, says, “There have been great strides and advances in testing for hereditary cancer.” With expanded testing, though, scientists see some new complexities in these diseases.
Breast cancer in the spotlight
Among all diseases, breast cancer is one of the most widely known and most common. The American Cancer Society reported that, in 2020, “female breast cancer has surpassed lung cancer as the most commonly diagnosed cancer.” Last year, 2.3 million women around the world received a breast-cancer diagnosis.
In addition, germline genes can play a fundamental role in breast cancer. Elena Stoffel and John Carethers, both at the University of Michigan Medical School in Ann Arbor, called breast cancer one of the most prevalent among hereditary cancers.
In the late 1990s, scientists connected changes in the breast cancer genes, BRCA1 and BRCA2, with an increased risk of this disease. By design, these genes play a role in repairing DNA, even suppressing tumors. With a harmful variant of BRCA1 or BRCA2, a woman’s risk of breast cancer rises. The U.S. National Cancer Institute (NCI) points out that “the degree of increase varies depending on the mutation.”
On average, about 2 out of 15 women develop breast cancer. Among women with a harmful variant of BRCA1 or BRCA2, that number could reach as many as 11 out of 15, according to the NCI. As will be discussed below, there’s more to hereditary breast cancer than the BRCAs.
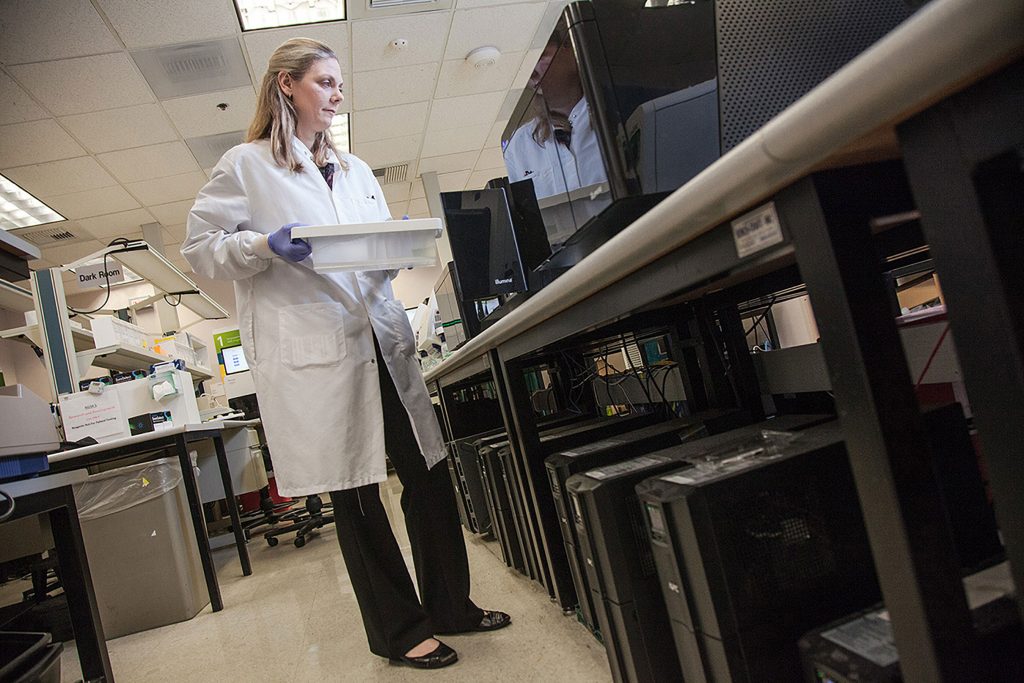
Simplifying and strengthening the testing
Today’s testing for hereditary cancer can be described in one word—easier. It’s easier right from the start with getting a sample. Instead of drawing blood, saliva testing is enough to test for some hereditary cancers. But that’s just the beginning of the simplification.
“In the past, physicians and their patients had to hop from lab to lab due to a lack of comprehensive offerings, to the genetic counselor and then back to bedside—often making the process of diagnosing hereditary cancer time-consuming, confusing, and costly,” says Fesko. Instead, today’s patients can get testing and an explanation of the results all in one place, such as a commercial testing lab.
These tests also provide more information. “As the science evolves, advancement in next generation sequencing provides the opportunity to give healthcare practitioners access to larger, guideline-based panels,” Fesko explains. “These panels allow them to test for many genes at once and then integrate the findings into treatment decisions.” That testing can also support opportunities to use some of the most advanced gene-targeted therapies. “Without advances in testing, this would not be possible,” he says.
That testing now goes beyond genes. “One exciting new avenue in hereditary cancer testing is the pairing of DNA sequencing with RNA analysis,” says Sarah Witherington, director of global product management, hereditary genetics at QIAGEN Digital Insights. “Adding RNA analysis can help laboratories by adding a new line of functional evidence when evaluating a variant of unknown significance.”

Even tests just for inherited cancers might not be enough. “In hereditary cancer, you must ensure that you’re doing appropriate germline testing, but it might still be important to do somatic tumor testing, as well,” Reddy says. He provides an example of a patient with ovarian cancer who does not know whether a hereditary cancer syndrome is driving it, but she only gets germline testing. If her germline testing for BRCA1 and BRCA2 came back negative, that should presumably rule out a hereditary cancer syndrome but it does not completely rule out that her tumor is being driven by a BRCA1 or BRCA2 somatic mutation. If it is, her therapy options would change. So, Reddy emphasizes, “That patient should also have somatic testing done on her tumor.”
In general, oncologists want more data on a patient. By adding more approaches to testing, clinicians might find hereditary cancers that would have been missed. “There is still a lot to learn in this space, and there are challenges to implementing DNA plus RNA testing as a standard of care, but it’s exciting to think about the possibilities,” Witherington says.
Reassessing the risk
All the data in the world about hereditary cancer is good for naught, unless someone knows what the numbers mean. In short, what’s the risk?
That’s not so easy to say. Even with BRCA variants, the risk of various cancers covers quite a range. It takes a genetic counselor to help sort out the results. “As oncologists turn to larger test panels, genetic counselors can really help with clinical interpretation and additional cancer risks,” Fesko says. “They can also provide insights on how mutations could manifest in a patient’s family members.” In some cases, testing related family members could reveal unknown cancer risks, such as a pathogenic variant being transmitted from one generation to the next.

These risk assessments apply to many cancers. For example, Witherington says: “There are two places in oncology where assessing risk for a hereditary cancer syndrome has recently become extremely important, and that is in prostate and pancreatic cancer.” She notes that recent clinical trials revealed variant-based treatments that can be effective in these cancers. “Appropriately assessing risk for hereditary cancer syndromes is becoming more intrinsically linked with treatment options for patients, so I expect this trend to continue and that we will see additional drugs and indications for these patients,” she explains.
Metabolic impact
A broad range of physiological processes can be impacted by cancer. In 1924, for example, German physiologist Otto Warburg found metabolic abnormalities in cancer cells. Today, genetic testing dives much deeper into this cancer connection.
From the University of Cambridge’s Medical Research Council’s Cancer Unit, research associate Marco Sciacovelli and his colleagues wrote that “it has been possible to identify a wide spectrum of heterozygous mutations in metabolic genes that may predispose to hereditary cancer.” Here’s how that could work: A person inherits a mutated and a wild-type allele, but loses the latter through, for example, chromosomal deletion, and that leads to a metabolism-related hereditary cancer.
Sciacovelli and his colleagues looked at heterozygous mutations involved with two enzymes—fumarate hydrase and succinate dehydrogenase—that contribute to the tricyclic acid cycle, which is central to producing fuel in the form of ATP, adenosine triphosphate. Inherited mutations in these enzymes lead to high levels of fumarate and succinate, respectively. Patients with these heterozygous mutations can also develop various cancers, such as rare ones like renal-cell cancer.
The breadth of potential metabolic impacts and disparate cancers reveal the range of hereditary connections. Learning more will require further investigation.
Expanding the reach
How far should oncologists look for hereditary cancers that might impact just one of 10 patients? “There was a time when the clinical utility of larger gene panels was debated,” Fesko says. Some clinicians still prefer tests based on a focused panel of gene variants, but other oncologists are looking bigger. “There are more genes that impact a diagnosis and treatment than previously understood,” Fesko says.
For example, more than BRCA variants impact hereditary breast cancer. A recent study by the Breast Cancer Association Consortium, for example, sequenced 34 genes in more than 60,000 and 50,000 women with and without breast cancer, respectively. The results showed strong correlations between breast cancer and variants in nine genes, including BRCA1 and BRCA2. The results also showed that some variants correlated more closely with specific types of breast cancer, such as estrogen receptor–positive disease.
As Witherington explains it: “The Breast Cancer Association Consortium study provided data that will help us to more accurately define a patient’s risk level for having breast cancer in association with certain genes as well as possibly predicting what subtype of breast cancer a patient may develop. These findings will help clinicians continue to tailor medical management, in accordance with national guidelines, for patients based on their genotype—hopefully leading to better outcomes.”

There’s no doubt that today’s advanced tests for hereditary cancer provide more information, but it’s just as clear that more must be known to make the most of the results. Recently, Holly LaDuca, associate director of clinical research at Ambry Genetics, and her colleagues studied 32 genes that can predispose people to hereditary cancer. This study examined 165,000 patients who were referred for multigene panel testing. The authors reported: “We identified extensive genetic heterogeneity surrounding predisposition to cancer types commonly referred for germline testing (breast, ovarian, colorectal, uterine/endometrial, pancreatic, and melanoma).”
The study also revealed some of the genetic complexity of cancer. As an example, in patients who met the current criteria to be tested only for BRCA1 and BRCA2, 67% of the pathological variants actually came from other genes. Based on this result and others, LaDuca and her colleagues encourage testing criteria to “include a broader spectrum of cancer predisposition genes.”
Beyond expanding the kind of testing, it should be available to more people. “We don’t want to miss traditionally underserved populations that aren’t getting access,” Reddy explains. Plus, different ethnic groups could face different risks. As an example, Reddy points out the black males have worse outcomes from prostate cancer than white males. “We need to leverage today’s tools to make sure that all patients have access to the testing they need.”
Accepting the complexity
Scientists learned long ago that the simplest explanations don’t always turn out to be the most accurate in genetics. In 1941, for example, American scientists George Beadle and Edward Tatum proposed the one gene-one protein hypothesis. The human genome includes fewer than 25,000 genes that code for proteins, but there are lots more proteins, maybe as many as 400,000—no one knows for sure. The point is just that genetics often get more complicated as scientists look more closely, and hereditary cancer is unlikely to be an exception.
Much like the number of human genes not correlating with the number of proteins, one variant in an inherited gene likely fails to reveal a person’s overall risk of cancer. A more complex problem requires more sophisticated analysis. For example, machine-learning expert Hamid Behravan at the University of Eastern Finland and his colleagues recently described a computational method of assessing breast-cancer risk—based on genetic variants, family history, and gene-interaction analysis—and they concluded that “demographic risk factors are individually more important than genetic variants in predicting” breast-cancer risk.
In other words, hereditary cancer is complicated. Every improvement in understanding that complexity, however, adds to the information that can be used to prevent or treat these diseases. It’s going to take a holistic approach—testing, sophisticated analysis, treatment, and deterrence where possible—to help the most people.
Will health experts ever recommend hereditary-cancer testing for everyone? When asked, Reddy says, “It’s complicated, but I believe that access to broad genetic/genomic testing is important as a public-health measure.” The more that oncologists learn about cancer—hereditary and non-hereditary—the better oncologists can treat individual patients. “The population health dynamic will shape our understanding of how to set up guidelines and quality measures as a society, and that will trickle down to an individual patient with a hereditary syndrome,” he says.
So, as more people get tested for hereditary cancer, scientists will learn more about these diseases.
Getting there, though, depends on making the best use of the data. As Reddy describes it: “Through data-driven clinical and lab insight and access to comprehensive high-quality testing, we’ll dramatically improve overall oncology care and improve the quality of life for more patients.”











