Thyroid dysfunction following cancer treatment with immune checkpoint inhibitors is more common than previously thought, according to research accepted for presentation at the Endocrine Society’s annual meeting (which was cancelled), and soon to be published in a special supplemental section of the Journal of the Endocrine Society.
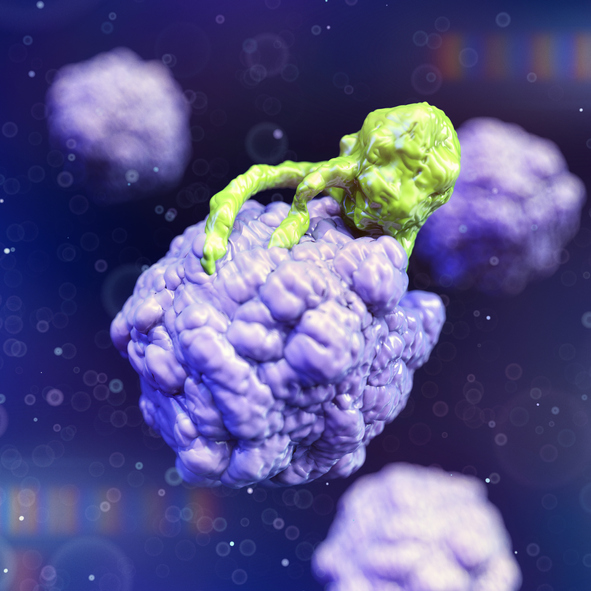
Cancer immunotherapy, particularly treatment with immune checkpoint inhibitors, has become an important part of treating some types of cancer and offers sustained remissions to those patients who respond, including those with cancers previously deemed untreatable. Immune checkpoint inhibitors take the ‘brakes’ off the immune system, which helps it recognize and attack cancer cells. Immune checkpoint inhibitors are approved to treat patients with a variety of cancers, including breast, bladder, cervical, colon, head and neck, liver, lung, skin, stomach, and rectal cancers. The market for these drugs is expected to reach more than $125 billion over the next few years.
Unfortunately, only a handful of patients benefit from these drugs, which are also very expensive. A recent analysis showed that the number of U.S. patients eligible for checkpoint inhibitor drugs increased from 1.54% in 2011 to 43.63% in 2018. The percentage of patients estimated to respond to checkpoint inhibitor drugs was 0.14% in 2011 and increased to 12.46% in 2018. (JAMA, May 3, 2019).
Along with the benefits of these treatments, possible side effects include immune-related adverse events, when the immune system attacks normal, noncancerous cells. One of the more common, but mild, side effects is abnormal thyroid levels, particularly hypothyroidism (an underactive thyroid).
“It was unclear to what extent this side effect occurred outside the clinical trial setting and so we used information from electronic health records to determine how common it was in practice,” said lead researcher Zoe Quandt, M.D., of the University of California, San Francisco in San Francisco, Calif. “Understanding who gets these immune-related adverse events, why they get them and what impact they have on response to therapy is an essential part of optimizing our use of immune checkpoint inhibitors.”
The researchers analyzed electronic health record data from the University of California, San Francisco on every patient who had received immune checkpoint inhibitors for treatment of cancer between 2012 and 2018.
They excluded anyone with thyroid cancer, whether or not that was the indication for the immune checkpoint inhibitor, or pre-existing thyroid disease. For the remaining 1,146 patients, they looked for those who had some type of thyroid dysfunction–either abnormal levels of thyroid hormones or a prescription for thyroid medication. Melanoma was the most common cancer treated (32%), followed by non-small cell lung cancer (13%).
Overall, 19% of subjects exposed to immune checkpoint inhibitors developed thyroid dysfunction. In contrast, a review of clinical trials found a much lower rate–6.6% of immune checkpoint inhibitor patients developed hypothyroidism, and 2.9% had hyperthyroidism, or an overactive thyroid.
The new study found thyroid problems varied by the type of cancer. The rate of thyroid dysfunction ranged from 10% of patients with the brain tumor glioblastoma to 40% in renal cell cancer, a type of kidney cancer. While there was no significant association between thyroid dysfunction and specific immune checkpoint inhibitors, thyroid dysfunction was more common in patients who received a combination of nivolumab (Opdivo) and ipilimumab (Yervoy) (31%) compared with either pembrolizumab (Keytruda) (18%), nivolumab (18%) or ipilimumab (15%) alone.













