Adding the immunotherapy blinatumomab after an initial round of consolidation chemotherapy in patients with good prognosis with B lineage acute lymphoblastic leukemia (ALL) kept most patients in remission and improved survival. Results of the randomized Phase III study showed that after three-and-a-half years of follow up, 83% of patients who received this combination therapy were still alive versus 65% who had received chemotherapy alone.
The results of the Phase III study E1910 were presented today at the American Society of Hematology (ASH) Annual Meeting and Exposition in New Orleans.
“The addition of blinatumomab to consolidation chemotherapy represents a new standard of care for patients with newly diagnosed B lineage acute lymphoblastic leukemia, who are in remission and have no measurable residual disease after induction chemotherapy,” said Mark R. Litzow, MD, a professor of medicine at the Mayo Clinic in Rochester, Minnesota.
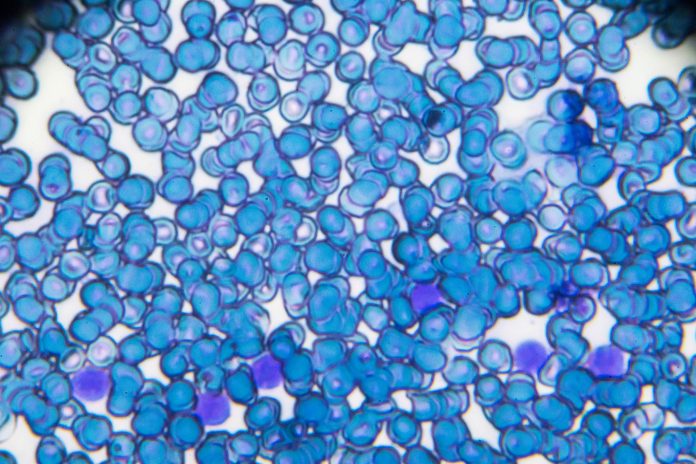
The goal of the trial was to improve the survival of patients with a better survival prognosis, defined as patients in completed remission and measurable residual disease (MRD) negative (<0.01%) by moving blinatumomab (trade name BLYNCITO, from Amgen) to a front-line treatment setting. Blinatumomab was first granted a Breakthrough Therapy Designation by the FDA in 2014 for for adults with Philadelphia-negative (Ph-) relapsed/refractory B-precursor ALL. This approval was expanded in 2018 to include children and adults with B-cell ALL who are in remission but still have measurable MRD. Amgen call the drug a bispecific T cell engager (BiTE®) targeted to recognize malignant B cells and destroy them.
The Phase III study was conducted between December 2013 and October 2019 at 77 sites throughout the U.S., Canada, and Israel. It enrolled 488 patients with newly diagnosed B lineage ALL with ages ranging from 30 to 70 and a median age of 51. The treatment followed a the complicated standard treatment of ALL as follows:
- Step 1—Induction. All participants received two and a half months of combination chemotherapy, including pegaspargase for those under age 55. Patients who tested positive for the B-lymphocyte antigen CD20 also received rituximab. At the end of induction, 395 patients (81%) were in remission, and 333 moved on to Step 2. The rest went off the study.
- Step 2—Intensification. Patients received a course of therapy to stop leukemia from developing in the central nervous system, a common site of relapse if not prevented. Then, all patients were tested centrally for MRD. While the primary evaluation was in the MRD- cohort, MRD+ patients continued in the trial.
- Step 3—Experimental. 286 patients (224 MRD- and 62 MRD+) were randomized/assigned to receive four cycles of consolidation chemotherapy with or without blinatumomab. Blinatumomab was given by continuous intravenous infusion for four weeks for each of the four cycles where it was provided. 72% of patients received blinatumomab by 72-and 96-hour infusions, which overcame feasibility issues for conducting the trial. Following FDA approval of blinatumomab for MRD+ patients in March 2018, MRD+ participants were assigned to the blinatumomab arm. MRD- patients continued to be randomized.
- Step—4 Maintenance. Patients received POMP therapy (Purinethol + Oncovin + methotrexate + prednisone) for about two years, commonly given to keep ALL in remission and increase the chance of achieving a cure.
An interim analysis—median follow-up time 43 months—showed that there were 56 deaths among the 224 MRD- patients, 17 in the chemotherapy plus blinatumomab arm and 39 in the control chemotherapy arm. Median overall survival was not reached in the chemotherapy plus blinatumomab arm but was nearly six years (71.4 months) in the control arm, with the trial continuing to follow the enrolled patients.
”This is the first randomized trial to demonstrate that we are able to improve the survival of ALL patients who are in complete remission, including by sensitive MRD testing, and establishes the addition of blinatumomab immunotherapy to standard consolidation chemotherapy as the new standard of care,” said Selina M. Luger, MD, chair of the ECOG ACRIN Leukemia Committee and a professor of medicine at the UPenn’s Abramson Cancer Center in Philadelphia.
Study E1910 was designed and conducted independently from industry with public funding. The ECOG-ACRIN Cancer Research Group (ECOG-ACRIN) led the trial with funding from the National Cancer Institute (NCI).













