An in-depth project mapping cancer-causing gene mutations to their encoded proteins and also tracking protein-protein interactions in cancer has allowed University of California scientists to gain new insight into the complex mechanisms of this disease, using head and neck cancer and breast cancer as specific examples.
Published as three papers in the current issue of Science and led by researchers Trey Ideker, University of California San Diego (UCSD), and Nevan Krogan, University of California San Francisco (UCSF), the project used proteomic mass spectrometry and also computer-based data integration to map linked proteins found in cancer cells. They also used a statistical model of mutation to assess which proteins are “under strong mutational selection and in which cancer types,” explain the authors.
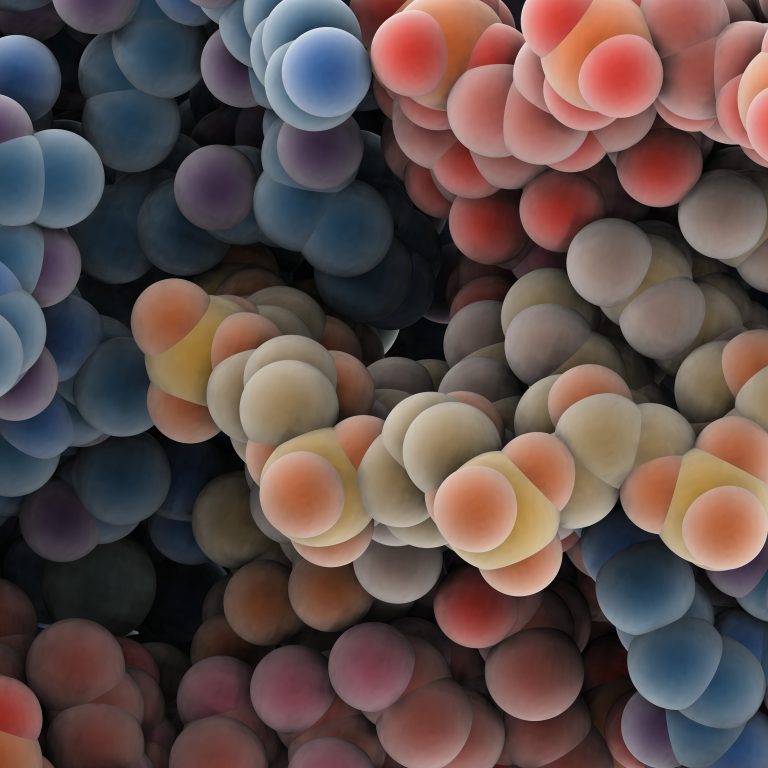
“We’re elevating the conversation about cancer from individual genes to proteins, allowing us to look at how the varying mutations we see in patients can have the same effects on protein function,” said Ideker in a press statement. “We’ve produced the first map looking at cancer through the lens of interactions between proteins.”
This approach and two of the current studies, which have a focus on breast cancer and head and neck cancer, all form part of a bigger project called the Cancer Cell Map Initiative (CCMI). This initiative, run jointly by UCSF and UCSD, is aiming to map and investigate all the molecular networks that lie behind cancer with a view to improving clinical decision making and treatments.
A small number of genes known to be mutated in cancers are already used as biomarkers by clinicians to predict a patient’s prognosis, or whether certain types of therapy will be effective, but these are relatively simple and fairly limited in number. The researchers behind the CCMI think mapping protein interactions could lead to more biomarker options.
“The problem is that we’ve only found a few genes that we can work with in this way to help guide prescription of an FDA-approved drug,” said Ideker. “Our studies provide a new definition of biomarkers based not on single genes or proteins but on the large, multi-protein complexes.”
The CCMI researchers mapped the networks of proteins formed by around 60 genes that are known to be pathogenic in breast cancer or head and neck cancers in both healthy cells and in two cancerous cell lines.
Around 79% of the protein-protein interactions in the breast cancer study had not previously been identified, and most (81%) were not shared across cell lines showing considerable variation occurs across cell types.
A number of new findings were revealed by the study, for example, the proteins BPIFA1 and SCGB2A1 were shown to act as negative regulators of the PI3K-AKT pathway in several breast cancers. The protein UBE2N was also shown to regularly interact with BRCA1.
Similarly, in the head and neck cancer study 84% of protein interactions were previously unknown. An interesting finding revealed by the study was that “PIK3CA mutant interaction specificity can determine the in vivo response to HER3 inhibitors,” write the authors, who add that PIK3CA helical domain variants seemed to make these cancer cells more sensitive to HER3 inhibitor drugs.
These studies are just the first steps towards mapping protein interactions in many cancer types, according to the researchers.
“We’re not only making connections between different genes and proteins but between different people and different disciplines,” Krogan said. “We’re in the perfect position to take advantage of this revolution on every level… I couldn’t be more excited than I am right now. We can do such damage to cancer.”













