The unfortunate reality for most cancer patients is that they will face resistance to one or more chemotherapeutic agents prescribed to eliminate their disease. Even more problematic, once a patient’s tumor is resistant to one type of chemotherapy, it is much more likely to be resistant to other chemotherapies as well, a conundrum long known as multidrug resistance. Once patients reach this point, the prognosis is often poor, and for the last 35 years, scientists have attempted to understand and block multidrug resistance in cancer by using experimental medicines. Interestingly, new data from investigators at Scripps Research in Florida suggests that this may not be the best approach.
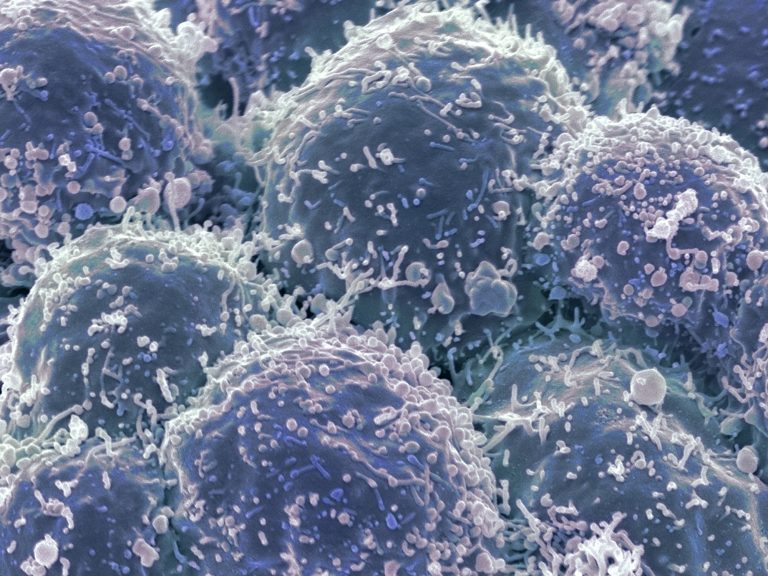
Inhibiting the key gene involved in cancer drug resistance has unintended side effects on specialized immune system cells called CD8+ cytotoxic T lymphocytes (CTLs), the team found. This could dull anti-cancer immune responses, and potentially increase vulnerability to infection since CTLs are “killer” T cells, essential in the fight against both viral and bacterial infections and tumors.
The findings from this new study—published recently in The Journal of Experimental Medicine through an article entitled “Physiological expression and function of the MDR1 transporter in cytotoxic T lymphocytes”—suggest that the repeated failure of MDR1 inhibitors in human cancer trials may be due to a previously unrecognized, and essential, function of the multidrug resistance-1 (MDR1) gene in CD8+ cytotoxic T lymphocytes.
Several genes are now recognized for contributing to multidrug resistance in cancer, but the first and most prominent of these is MDR1. Its discovery more than three decades ago set off a race to develop drugs that would inhibit the expression of MDR1. But those MDR1 inhibitor drugs have consistently disappointed in clinical trials. The reasons behind these failures have remained enigmatic.
“MDR1 acts as a chemotherapeutic drug efflux pump in tumor cells, although its physiological functions remain enigmatic,” the authors wrote.
“Using a recently developed MDR1-knockin reporter allele (Abcb1aAME), we found that constitutive MDR1 expression among hematopoietic cells was observed in cytolytic lymphocytes—including CD8+ cytotoxic T lymphocytes (CTLs) and natural killer cells—and regulated by Runt-related (Runx) transcription factors,” the authors penned. “Whereas MDR1 was dispensable for naive CD8+ T cell development, it was required for both the normal accumulation of effector CTLs following acute viral infection and the protective function of memory CTLs following challenge with an intracellular bacterium. MDR1 acted early after naive CD8+ T cell activation to suppress oxidative stress, enforce survival, and safeguard mitochondrial function in nascent CTLs.”
Considering that these cells are also necessary for warding off most cancerous tumors, blocking MDR1 with existing inhibitors could also cripple natural immune responses to cancers.
“With the help of our collaborators at New York University Medical Center, we looked at mouse immune cells from five major lymphoid and nonlymphoid tissues: bone marrow, thymus, spleen, lung, and small intestine,” explained senior study investigator Mark Sundrud, PhD, associate professor of Immunology and Microbiology at Scripps Research. “It became clear that the types of cells that are key to fighting infections and cancers are among those most sensitive to blocking MDR1 function.”
It has been known for decades that CTLs, as well as “natural killer” cells, a type of white blood cell, express high levels of the MDR1 gene. But because MDR1 has historically been viewed only through the lens of creating multidrug resistance in cancer cells, few researchers thought to ask what MDR1 does during normal immune responses; those that did found confusing and often contradictory results, Sundrud says, likely due to the use of non-specific animal model systems.
Convinced that MDR1 might impact natural immune responses, Sundrud and his colleagues sought to devise more specific mouse models to directly visualize and functionally characterize MDR1 expression in vivo. Additional experiments revealed that blocking MDR1 function hampered the earliest stages of the CTL response to infections when these cells multiply rapidly to reach the numbers needed to kill all viral and bacterial invaders. In line with this result, MDR1 inhibition also affected long-lived immunity to infections that have been previously seen and eradicated. It also affected the cells’ energy organelles, called mitochondria.
“We think that MDR1 plays a special role in helping mitochondria provide energy to growing cells,” Sundrud remarked. “So, if you take this away, it makes sense that these cells can’t support the metabolic demand of cell division and that they ultimately die.”
On the one hand, the research raises questions about the safety and utility of using systemic MDR1 inhibitors as cancer therapies. At the same time, the work reveals important new mechanisms that determine how the immune system fights off infections and develops long-lived memory.
“These insights become all the more pertinent today, given all the questions and concerns related to immunity against the pandemic coronavirus that causes COVID-19,” Sundrud noted.
The team is now looking to use this new knowledge to finally nail down a unifying function of MDR1 in all cells, whether it is in CTLs responding to infections, or cancer cells trying to deal with chemotherapeutic agents.
In the shorter term, Scripps researchers plan to explore new approaches to re-design existing MDR1 inhibitors to specifically target only cancer cells.
“This way you might be able to prevent multidrug resistance in cancer cells, without affecting the immune cells that are trying to fight off the tumor,” Sundrud concluded.













