Traditional vaccines work by teaching the immune system to recognize a virus or bacteria that needs to be attacked. Now, researchers at the University of Chicago’s Pritzker School of Molecular Engineering (PME) say they have developed a new vaccine that does just the opposite by removing the immune system’s memory of one molecule, an “inverse vaccine” that could be developed to treat multiple sclerosis (MS) and a range of other autoimmune diseases.
The investigators from PME note that immune memory erasure would be an unwanted result for addressing infectious diseases, but achieving that effect for autoimmune diseases, where the immune system attacks a person’s health cells, could halt autoimmune reactions to treat not only MS, but potentially type 1 diabetes, rheumatoid arthritis, Crohn’s disease, and others. Their findings are published in the journal Nature Biomedical Engineering.
The new inverse vaccine uses the liver’s method for naturally marking molecules from broken down cells with markers that prevent autoimmune reactions to cells that die via natural processes. To create the vaccine, the PME team assembled an antigen (a molecule being attacked by the immune system), with a molecule that resembles a fragment of an aging cell that the liver would recognize as innocuous. Taking this approach they were able to demonstrate how the vaccine could successfully stop the autoimmune reaction associated with a MS-like disease.
“In the past, we showed that we could use this approach to prevent autoimmunity,” said Jeffrey Hubbell, a professor of Tissue Engineering and lead author of the new research. “But what is so exciting about this work is that we have shown that we can treat diseases like multiple sclerosis after there is already ongoing inflammation, which is more useful in a real-world context.”
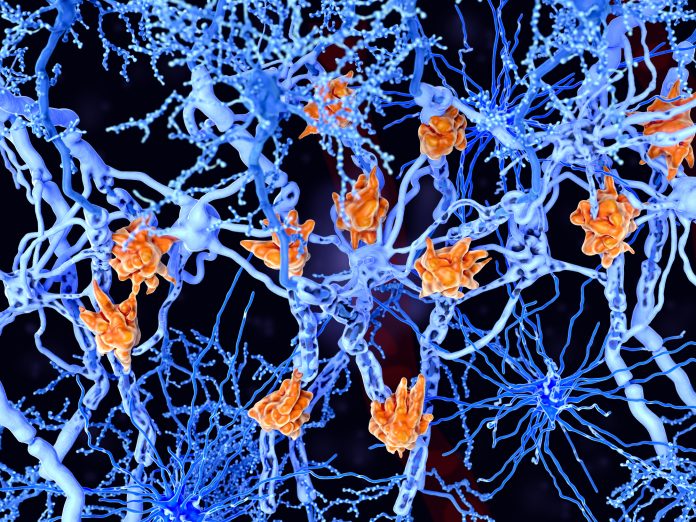
While the job of the immune system’s T cells is to recognize cells that are foreign to the body and eliminate them, sometimes these cells make mistakes and intend attack normal tissue in the human body. In the case of MS, T cells treat myelin—the protective covering around nerves—as foreign and attacks then; in Crohn’s disease the T cells attack cells in the small intestine.
To address this, Hubbell and colleagues looked to leverage the knowledge that there is not an immune response to every damaged cells in the body, this phenomenon is known as peripheral immune tolerance and is a process that occurs in the liver. In the past few years, the PME researchers have discovered that tagging molecules with the sugar known as N-acetylgalactosamine (pGal) mimics peripheral immune tolerance.
“The idea is that we can attach any molecule we want to pGal and it will teach the immune system to tolerate it,” said Hubbell. “Rather than rev up immunity as with a vaccine, we can tamp it down in a very specific way with an inverse vaccine.”
To study the effects of pairing pGal to another molecule, the PME team studied it in an MS-like disease by linking myelin proteins to pGal and found that the immune system stopped attacking myelin, which allowed the nerves to function properly and reversed MS symptom in an animal model. Further studies showed this approach worked to minimize other ongoing immune reactions.
The researchers note that an initial Phase I safety trial of the inverse vaccine approach has already been conducted in people with celiac disease and further safety trials are currently being conducted in people with MS. These trials are being conducted by the pharmaceutical company Anokion SA, which was co-founded by Hubbell.
The hope is that this new approach to treating autoimmune diseases can be more effective than current methods, which are broadly block immune response leaving patients susceptible to infections and other side effects.
“If we could treat patients with an inverse vaccine instead, it could be much more specific and lead to fewer side effects,” Hubbell said. “There are no clinically approved inverse vaccines yet, but we’re incredibly excited about moving this technology forward.”













