Researchers have learned that loss of just a single copy of the CDKNA/B genes speeds up the rate of recurrence in the most aggressive type of meningiomas, categorized as group C tumors. These meningiomas account for about 20% to 25% of all meningiomas, yet only a small fraction of 2-4% harbor loss of one or two copies of the CDKNA/B genes. Nearly all these patients recur immediately after neurosurgery.
In a study published in Acta Neuropathologica, researchers from Baylor College of Medicine found that these patients with CDKNA/B loss have a poor prognosis compared with all meningiomas, including others of the group C molecular classification, and relapse almost immediately after surgery.
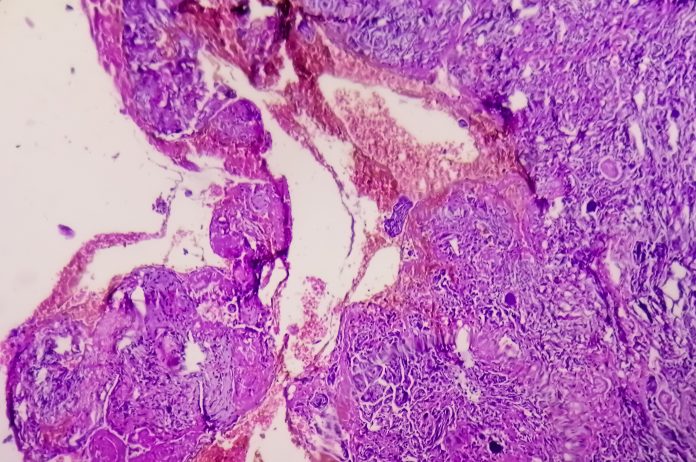
For decades, meningiomas have been classified by the World Health Organization (WHO) using histopathologic markers. But in the last several years, there has been a push in the meningioma field to try to see if there are molecular classes of meningiomas. In 2019, the Baylor team published a paper in PNAS which first identified three molecular groups: A, B, and C. Within the past year, two other research groups confirmed classification systems that validated Baylor’s.
Because of that, the WHO now includes molecular findings into its meningioma classification.
“WHO now states that if the meningioma tumor shows the loss of both copies of CDKN2A or B—or homozygous loss—the tumor should be classified as grade C tumor,” said co-senior author and neurosurgeon Akash Patel, MD, of the Jan and Dan Duncan Neurological Research Institute, Texas Children’s Hospital. To get to those results, WHO included several tests, including methylation profiling, which reveals gene loss.
In response, the team essentially repeated the WHO study, digging deeper into the molecular features of meningiomas using a variety of methodologies: methylation, RNA classification, and copy number/chromosomal loss. “We can now safely say that these three groups are biological groups,” adds Patel.
In the present study, the team examined 776 meningioma tumors of all grades obtained from patients enrolled at four different institutions. First, they graded them using 2016 WHO guidelines. Then, they used methylation and RNA seq profiling data to classify them as Group A, B, or C.
The team made a couple of discoveries. “First, the CDKN2A or B loss only happens in the most aggressive group, what we call Group C meningiomas, which we proposed were the worst acting meningiomas,” says Patel. These meningiomas exhibit chromosomal instability so it was not a shock they lost CDKN2A and B. “Second, we found that even heterozygous loss—the loss of one copy of CDKN2A or B—is just as bad,” Patel explained.
As expected, Group A and B meningiomas had no CDKN2A or B loss and about 75% of the patients did not relapse even after 15 years. But nearly half of patients with Group C loss relapsed within 47 months.
But when the team looked further into the group C meningiomas, they found that 50% of those with intact CDKN2A or B relapsed. “But the patients who had loss of one OR two copies of CDKN2A or B relapsed almost immediately, within 11 to 25 months or one to two years of surgery” said Patel.
These findings suggest that meningioma patients should first be identified with group C tumors and then look for CDKN2A or B loss—either homozygous or heterozygous—to help further refining the prognosis.
“As a neurosurgeon, if I was able to tell what kind of molecular group tumor a person had, especially if it was a group C tumor, I would be more aggressive at the time of surgery to get out as much as we possibly can,” Patel says.
Looking further, the Baylor College of Medicine team would like to initiate clinical trials to see if they can identify patients with aggressive group C tumors, especially those with CDKN2A or B loss, and test a few different approaches. One would be to evaluate radiation immediately after surgery, which is not currently standard of care. Another would be to start with radiation, followed by surgery.
“Part of the work that has hampered the progress in treating meningiomas is that we were working in murky waters,” said Patel. “And I think now that we’ve found these biologically relevant groups, we can understand the biology better and maybe propose and discover treatment paradigms that are specific to the biology of those tumors.” One long-term goal would be to see how these biological features funnel down on a molecular level. “Then, maybe we can pinpoint exactly what the bottom-line problem is and perhaps make targeted therapies directed towards that.”













