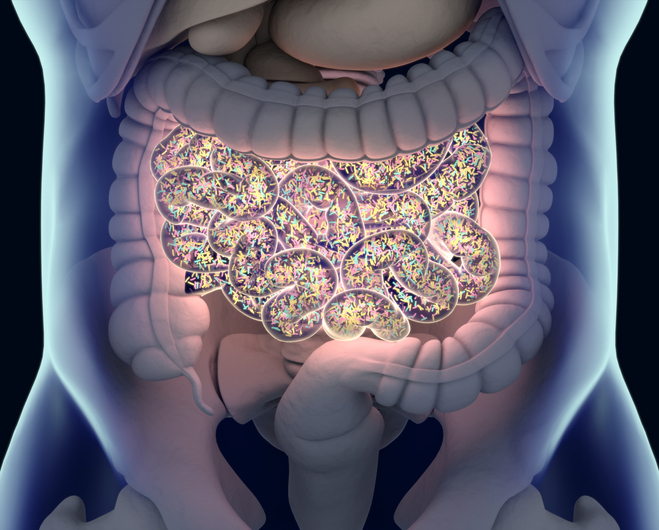
For bacteria in the gut, life can be nasty, brutish, and short—especially if they lack immunity factors that can protect them against the toxins released by other bacteria. These immunity factors, scientists based at the University of Washington have determined, can be acquired by one bacterial species from another.
The finding comes as something of a surprise. The scientists had thought that in any given bacterial species, toxin and immunity genes would come in pairs, rather like matching locks and keys, so that bacteria can avoid harming themselves or other bacteria of the same species. Yet genomic analyses of bacteria derived from the gut microbiome indicated that something more interesting was going on.
The scientists, led by Joseph D. Mougous, Ph.D., focused on a group of gut bacteria from the order Bacteroidales. These bacteria have a secretion mechanism to inject toxic proteins into bacteria that crowd too close. At the same time, they keep themselves safe from their own or their kin cells’ poisons by carrying specific immunity factors that neutralize the toxins.
According to the scientists, several Bacteroides species that populate the human gut have acquired sizable interbacterial defense gene clusters. These encode for large arrays of immunity determinants that neutralize the direct hit of toxins from their competitors. The clusters have features that suggest they are actively acquiring new immunity genes as new threats are encountered.
Detailed findings appeared October 30 in the journal Nature, in an article titled, “Human gut bacteria contain acquired interbacterial defense systems.”
After scrutinizing Bacteroides fragilis, a gut species known to produce many secreted toxins, the scientists saw, as anticipated, that genes conferring immunity to the B. fragilis toxins were found in many of the samples in relatively the same abundance as markers for the presence of that species. This finding suggested that these immunity genes are encoded by B. fragilis itself.
In other samples, however, the immunity genes appeared at substantially higher abundance than B. fragilis species markers. They were even detected in some microbiome samples without any B. fragilis.
“This finding strongly suggests that these anti-B. fragilis immunity elements were encoded by other bacteria in the gut,” the scientists explained. Using statistical analyses, the researchers concluded that these included B. ovatus, B. vulgatus, B. helcogenes, and B. coprocola. Looking at the genomes of these organisms, they discovered that they carried genes that would be expected to make them immune to toxins delivered from B. fragilis. Moreover, in the genomes, these immunity genes were located in large clusters together with other immunity genes predicted to protect against other B. fragilis toxins.
“The clusters reside on mobile elements,” the article’s authors added, “and their transfer is sufficient to confer resistance to toxins in vitro and in gnotobiotic mice.”
When the researchers mixed together a bacterium that carried one of the clusters with a related organism that did not have one, they learned that the immunity genes could be transferred, and that the newly acquired genes did offer toxin protection.
Based on their observations, the scientists think these immunity genes have an adaptive role because they help these bacteria overcome toxic hits from their B. fragilis assailants. They see this shielding effect during growth in Petri dishes in their labs and when they introduced the bacteria carrying these genes into the guts of mice.
“Finally, we identify and validate the protective capability of a recombinase-associated AID subtype (rAID-1) that is present broadly in Bacteroidales genomes,” the scientists noted. “These rAID-1 gene clusters have a structure suggestive of active gene acquisition and include predicted immunity factors of toxins derived from diverse organisms.”
Essentially, the scientists discovered a second set of orphan immunity gene clusters that are widespread among Bacteroides species in the gut. These clusters contain genes predicted to guard against diverse toxins made by a range of different species, not just other Bacteroides. A second striking feature of this second kind of immunity gene cluster is that it shows signs of recent new gene acquisition.
The scientists concluded that obtaining and maintaining orphan immunity genes clusters is a common way for gut bacteria to try to fend off interbacterial assaults and sustain their species’ or strain’s presence in the human gut microbiome.
What’s more, it appears that human fecal samples have unique combinations of toxin and immunity genes. “So, what it takes to survive in one person’s microbiome might not be the same in another person’s microbiome,” Mougous observed.
The results could help explain why it’s so hard for people to tinker with their microbiome compositions. “Generalized approaches for colonizing the gut with certain bacteria may never succeed,” he continued. “[Colonization approaches] may need to be individualized.”











