Using techniques inspired by next generation sequencing, Austrian scientists have developed a SARS-CoV-2 testing method that retains the accuracy of RT-PCR but can process up to 36,000 samples in less than 48 hours.
Although vaccine campaigns are ramping up in many countries and at least some places around the world are starting to get back to normal, the COVID-19 pandemic is still very much with us. Having reliable and efficient testing systems in place is therefore likely to be a requirement for some time to come.
A lot of countries have adopted antigen testing as an everyday method as it is cheap, quick and easy. However, it is one of the less sensitive testing methods, as a reasonably high amount of viral particles are needed to trigger a positive result, and there remains a danger that asymptomatic individuals may not be detected and go on to spread to virus to others.
In contrast, RT-PCR is very accurate but time consuming and costly. Pooled PCR testing is being rolled out in some places to make testing more efficient, but this comes with some problems as if one sample in the group is positive then everyone included in that pool has to be retested.
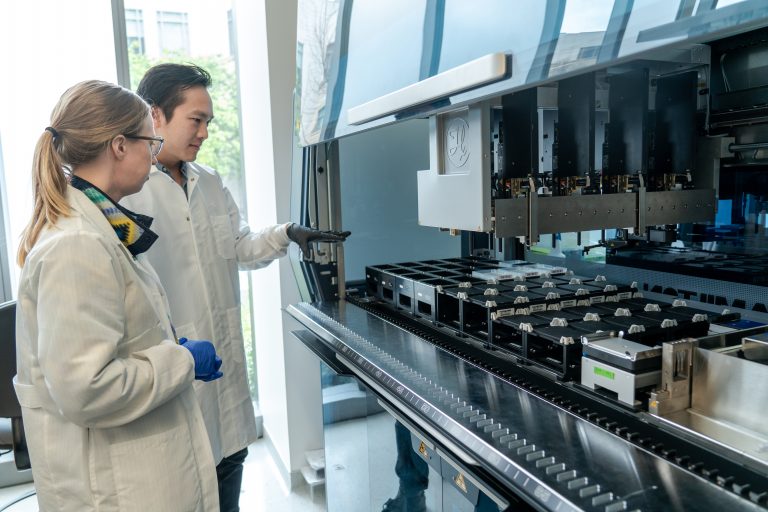
To combat this problem, the researchers created a system called saliva analysis by RNA sequencing or SARSeq that has the same accuracy as PCR, but can process thousands of samples quickly and also identify individual samples. The method used is similar to that applied in next generation sequencing.
The process starts by each patient sample being added to an individual well on a 96-well testing plate. Then any well containing a specific viral sequence is detected and amplified by PCR. At the same time each sample containing viral particles is identified by a unique DNA barcode to enable individual samples to be identified.
In the second step, all the samples from the first plate are pooled and a second DNA barcode added that will attach to positive samples. This second marker allows the samples to be pooled a second time and still identified later.
“We combine the sensitivity of PCR with the high throughput of Next Generation Sequencing technology, or NGS, the same used to sequence the human genome. The NGS machine processes the pooled samples and tells us which samples contained any SARS-CoV-2 material. The barcodes allow us to distinguish each positive sample from the others, and trace it back to a patient,” says Ramesh Yelagandula, Ph.D., a researcher at the Institute of Molecular Biotechnology of the Austrian Academy of Science (IMBA) based at the Vienna BioCenter. Yelagandula is first author of the paper describing the research published in Nature Communications.
After several rounds of testing across different human samples and a comparison to gold standard RT-PCR the team concluded that the SARSeq method was able to pick up even low levels of SARS-CoV-2 in samples. Cycle threshold (Ct) is a measure used to determine whether a test is positive or not. For SARS-CoV-2 a Ct value less than 40 has been widely reported as positive with lower numbers indicating higher numbers of viral particles present in a sample. The SARSeq test was able to detect Ct values of 36 and even up to 39, although samples in the 36-40 range were less likely to be detected.
The team also tested the potential for SARSeq to distinguish between SARS-CoV-2, two strains of influenza A and three strains of rhinovirus and found it was able to do so with a high level of accuracy. No false positives were detected and only a small number of false negatives when the dilution of virus was in the 30-40 Ct range.
“We developed SARSeq to try and circumvent the limitations of other tests, and to process thousands of samples in parallel. Not only is it an excellent method to detect SARS-CoV-2, but it can also be applied to other respiratory pathogens like the flu virus, the common cold rhinoviruses, and potentially many others,” says Ulrich Elling, Ph.D., a group leader at the IMBA who co-led the project.













