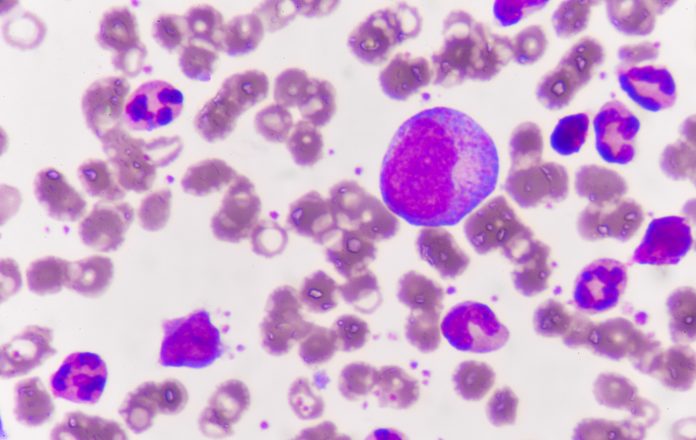
U.S. researchers at the University of California in Irvine have developed a mathematical model that they believe can help predict treatment response in patients with the white blood cell cancer chronic myeloid leukemia.
The model identified patients most likely to respond well to treatment with tyrosine kinase inhibitors (TKIs) and also suggested a combination therapy that could overcome primary resistance.
A key predictor of reduced TKI response was the increased tendency of hematopoietic stem cells to self-renew, which in turn influenced the self-renewal of leukemic stem cells.
In addition, an increase in the proportion of chronic myeloid leukemia stem cells in the bone marrow indicated a decreased likelihood of the disease responding to TKI therapy.
“The model predicts that stimulating the differentiation of leukemic stem cells while applying TKI therapy can significantly improve treatment outcomes,” report Jonathan Rodriguez, from the Center for Complex Biological Systems, and colleagues.
The findings are published on the bioRxiv preprint biology server, ahead of formal journal publication.
TKIs have proven effective for the chronic myeloid leukemia but there remain patients who do not respond to treatment even if they do not carry mutations that mediate drug resistance.
To discover novel strategies to improve TKI therapy outcomes, the team developed a nonlinear mathematical model of the formation of blood cell components in a healthy scenario and that of chronic myeloid cancer.
This incorporated feedback control and lineage branching, with cell-cell interactions modulated by previous data and new murine studies.
The resulting model captured the dynamics of normal and cancer cells at various stages of the disease and exhibited variations in TKI treatment response consistent with that seen in patients, the researchers note.
“In summary, the feedback/feedforward model we have presented here, while a simplified version of normal and [chronic myeloid leukemia] hematopoiesis, makes novel and testable predictions regarding the origins of non genetic primary resistance, which patients will respond to TKI treatment and suggests a combination therapy that can overcome primary resistance,” they report.
“Although preliminary evidence was presented to support model predictions, future work should focus on designing targeted experiments and collecting patient outcomes to generate data to more thoroughly test the model.”













