Targeted radiation with stereotactic radiosurgery (SRS) may be as good as whole brain radiotherapy (WBRT) for the treatment of brain metastases in people with small-cell lung cancer (SCLC), suggest results of a meta-analysis carried out by researchers from the University of Toronto in Ontario, Canada.
The findings challenge previous concerns regarding the use of SRS in these patients given their perceived risk of rapid intracranial progression, said the investigators.
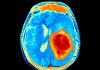
At present WBRT is the standard-of-care for people with intracranial metastatic disease (IMD) that is secondary to SCLC, but the treatment can be associated with acute, subacute, and delated adverse effects. While the acute and subacute reactions, such as fatigue, hair loss, skin rashes, and short-term memory loss are generally thought to be reversible, delayed reactions, which occur more than 6 months after treatment are irreversible and progressive. These include demyelination of nerve cells, vascular abnormalities, and tissue death that together can lead to cognitive impairments.
“Since patients with SCLC have traditionally been predicted to have a short overall survival [OS], the benefits of WBRT in its ability to treat brain metastases and prevent neurocognitive effects secondary to IMD have previously been thought to outweigh the risks of neurocognitive deterioration as a consequence of the radiation treatment itself,” said the study’s first author Karolina Gaebe, a medical student at the University of Toronto working under the supervision of Dr. Sunit Das at St. Michael’s Hospital.
“However, more recent estimates suggest that SCLC survival [has] improved as a result of treatment advances, calling this paradigm into question,” she told Inside Precision Medicine.
SRS is a targeted therapy that limits radiation exposure to healthy brain tissue and is associated with less central nervous system toxicity. It is the recommended first-line treatment for IMD arising from most solid cancers but trials that initially established its non-inferiority over WBRT excluded patients with IMD due to SCLC. Gaebe said the reasons for this were “multifactorial, but generally center around concerns over rapid intracranial progression in patients with SCLC.”
Therefore, evidence for SRS in patients with SCLC is currently based on observational studies that can be limited by their small sample size. In addition, a survey of radiation oncologists in the US showed that while many would consider SRS for patients with SCLC and limited brain metastases, rapid intracranial progression and a lack of high-level data are major concerns.
To address this, Gaebe and team carried out a meta-analysis of data from seven retrospective studies that compared treatment outcomes between SRS and WBRT in 18,130 patients with SCLC and IMD.
They found that SRS was associated with a significant 15% lower risk for death from any cause relative to WBRT with or without SRS. The difference was driven a significant 23% lower risk for death with SRS versus WBRT alone.
Conversely, there was no significant difference in OS between patients who received SRS and those who received WBRT with an SRS boost.
Pooled median OS among the participants who received SRS was 9.0 months, which the researchers point out is higher than the typical estimates of 4 to 6 months.
There was also no significant difference between the two treatments in the risk for intracranial progression. Median intracranial progression-free survival from first-line treatment with SRS was 4.9 months and the 12-month local and distant intracranial progression rates were 78% and 58%, respectively.
Gaebe says that the analysis highlights the lack of SRS data available in patients with SCLC and IMD and that her team are now in the early stages of planning a clinical trial. In addition, she notes that several other trials are currently enrolling patients to investigate SRS treatment in these patients.
These include the ENCEPHALON trial which will include SCLC patients with IMD (≤10 brain metastases) who have not received previous radiation therapy to the brain, have good performance status, and have no history of of toxicity from prior therapies and no other cancers diagnosed in the previous 5 years.
The authors conclude in the paper that their “findings indicate that at least a subset of patients with SCLC survive sufficiently long following SRS treatment to benefit from reduced neurotoxicity.”
In a statement to the press, Dr. Das, who was a senior author on the study, said: “Because this is a meta-analysis, we can’t use this as absolute evidence that all patients should be treated [with SRS]. But essentially, this means that we need to challenge our standing worldwide paradigms for treating patients with this disease and revisit the idea that these patients should receive whole brain radiation therapy.”