In the 1600s, Dutch microscope pioneer Antonie van Leeuwenhoek found various microbes—bacteria, fungi, and other microorganisms—on and in humans. Little did he know that nearly 350 years later, the collection of human microbes would be recognized as a key ingredient in human health. Today, this microbiome plays a role in research from cancer to neurodegeneration and many more with impacts on human health. As scientists learn more about the human microbiome’s role in disease, this information promises to improve human health.

Duke University
“We all have countless microbes that live in and on us and actually outnumber human cells,” said Neil Surana, assistant professor of pediatrics at Duke University. “Moreover, these microbes are essential for regulating health and preventing disease.”
The idea started with the hygiene hypothesis, Surana explained, which suggests “that inadequacies in microbial exposure—in combination with genetic susceptibilities—lead to a collapse of the normally highly coordinated immune response.” So, certain changes in the microbiome can make a person more or less susceptible to particular diseases. Plus, Surana noted, this comes along with “the idea that restoring the microbiota to ‘normal’ will help prevent or even treat disease.”
The composition and structure of one microbiome is not the same as another. That applies to one person’s microbiome in different places, say the gut verses the skin, as well as microbiomes between people. Some of the variables even extend beyond what might be expected (See “Gaps in the Gut”).
Not all new
Connecting microbes with medicine is not a new idea. Antibiotics, for example, address imbalances in the microbiome. “Although these are used most often to treat a specific infection, there are times when antibiotics are used for their anti-inflammatory effect rather than targeting a specific pathogen,” Surana said. “Although the basis for these anti-inflammatory effects was initially not understood, it is becoming more clear that this is related to altering the microbiome in a way that benefits the immune system.”
One thing that is newer in this arena is called a fecal microbiota transplantation (FMT). Perhaps less desirable than a prescription for antibiotics, FMT can be used to treat an ongoing infection with Clostridiodes difficile, which can evade the impact of antibiotics as it causes ongoing diarrhea. In this application, FMT tends to be very effective, but Surana notes a downside: “It has been associated with rare side effects including transmission of antibiotic-resistant pathogens.”
Some patients might be happy to hear that FMT is not the only microbiome-related approach to gastrointestinal challenges. With colitis, for example, Surana and his colleagues showed that Clostridium immunis—a relative of C. difficile—can protect mice from this digestive disease.1
Computation for colitis
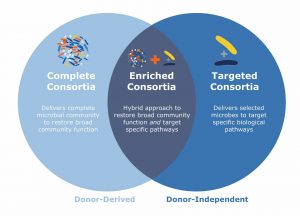
In Somerville, MA, scientists at Finch Therapeutics apply artificial intelligence to the development of microbiome-based therapeutics through its Human-First Discovery platform. This “platform leverages machine learning, data from human microbiota transplantation studies and molecular characterization, which we believe can be used to: identify diseases where addressing dysbiosis—a microbiome imbalance—provides therapeutic benefit; reveal the mechanisms that underlie these results; and uncover key microbes and functional pathways that drive these clinical outcomes,” said Sonia Timberlake, Ph.D., senior vice president of research at Finch. “We believe this reverse translation strategy is the optimal approach to developing microbiome therapeutics, providing causal insights that cannot be gleaned from preclinical in vitro or in vivo experiments alone.”

Finch Therapeutics
One of Finch’s therapeutics is in development as a treatment for ulcerative colitis. Using the Human-First Discovery platform, Finch scientists identified deficiencies in microbes and microbial functions in patients with this condition. “Target organisms were isolated directly from the specific donors whose samples induced response or remission in clinical studies of FMT for ulcerative colitis,” Timberlake says. From this work and in collaboration with Japan-based Takeda Pharmaceutical Company, Finch developed an investigational drug known as TAK-524, which “is composed of both spore-forming and non-spore-forming bacterial strains selected for the treatment of ulcerative colitis,” Timberlake explains. “TAK-524 is currently a preclinical-stage program.”
Searching for an anti-cancer community
Much like today’s personalized medicine invests heavily in cancer treatments, microbiome-based medicine could do the same, and this is not a new connection. Cancer surgeon and researcher Jennifer Wargo, of The University of Texas MD Anderson Cancer Center in Houston, and her colleagues wrote: “Historical accounts linking cancer and microbes date as early as four millennia ago.”2 Still, the connection between cancer and microbes proves difficult to document. As Wargo and her colleagues pointed out: “Few microbes directly cause cancer, but many seem complicit in its growth, often acting through the host’s immune system; conversely, several have immunostimulatory properties.”

The University of Texas MD Anderson Cancer Center
So, as molecular virologist Nadim Ajami, executive director of MD Anderson’s Program for Innovative Microbiome and Translational Research (PRIME-TR), noted: “You have good microbes that promote all aspects of health, and we also have the sort of bad bugs—some of which carry virulence factors that could promote the onset of cancer or carcinogenesis.”
Sometimes, scientists discover the connection between cancer and the microbiome by chance. For instance, Wargo calls her introduction to this area of research serendipitous. She was studying the resistance to a treatment for pancreatic cancer, and what she “found is that—in certain cell lines—they were actually contaminated with bacteria and the bacteria were creating or promoting resistance or helping the cancer to resist treatment with chemotherapy,” she says.
Today, she studies the impact of the gut microbiome on cancer. “The bugs in the gut of a patient going on cancer immunotherapy can dictate whether or not that patient responds, and you can actually change someone’s microbiome using a fecal transplant—believe it or not—and make them respond better to cancer therapy.” This work started with observations drawn from patients with melanoma undergoing immunotherapy treatment, and although it has now translated to a beneficial therapeutic effect there is more ground to cover ahead.3–5
Working together, Ajami said that he and Wargo are “trying to identify the impact of the microbiome on the onset of cancer, progression of cancer, and the response to therapy.” Ajami hopes that “one day we can devise strategies to intercept, or even prevent cancer.”
That will probably not depend on a single kind of microbe but likely on an ecosystem of many microorganisms. “We know that a healthy community promotes or provides a cancer patient with a better chance of responding to their treatment,” Ajami said. So far, it remains unclear exactly what makes up a healthy microbiome, and it probably varies between people. Still, there is clearly a beneficial overlap—some part of the functionality of the microbiome that is common among people and plays a role in good health.
If Wargo and Ajami can define the community of common microbes that are good for people, what can they do with it? “Could we get some kind of a universal signature or approach to modulate the microbiome that would promote overall health?” Wargo asks. “My hunch is yes, but it’s complicated, it’s gonna take a little while to get there.”
Connecting the mind and microbes
Microbes in a person’s gut impact the nervous system in several ways, according to Eran Blacher, Ph.D., postdoctoral research fellow in neurology and neurosciences at Stanford University. For one thing, metabolites produced by the bacteria get absorbed in the blood stream and reach the brain, “where they can modulate the activities of brain cells, such as neurons, astrocytes and microglia,” Blacher says. Bacteria and their metabolites in the gut can also trigger a more direct impact through the gut nervous system, which is connected to the brain. Plus, Blacher explains that “bacteria can interact with immune cells in the gut that can migrate from the gut, infiltrate the brain through the blood stream or secrete immune-related molecules—chemokines and cytokines—that can modulate brain-cell functions.”
Blacher describes the brain as a “fascinating new frontier” in health-related research on the microbiome, and his work on amyotrophic lateral sclerosis (ALS) makes an interesting example. “Understanding new mechanisms involved in ALS pathogenesis might serve as a potential treatment strategy,” he says. As an example, Blacher says that his postdoctoral research in immunologist Eran Elinav’s laboratory at the Weizmann Institute of Science in Israel revealed “that treatment with a single bacterium, Akkermansia muciniphila, significantly improved motor functions and ameliorated ALS symptoms in a mouse model of ALS.”6
Although a microbe-based treatment for ALS is a long way off, the microbiome can already be used in brain research. As Blacher says, “We can now utilize gut bacteria as biosensors or even predictors of their hosts’ metabolic state to identify and study interesting biological pathways involved in different phenotypes.”
Completing the translation
Despite the excitement around microbiome-based therapeutics, considerable work lies ahead. “The main hurdle for microbiome-based therapies is to identify a specific bacterium—and, ideally, its bioactive products—that can protect against the disease of interest, and that’s a challenging feat given the sheer number of microbes present in the microbiota,” Surana explained. “Having this bacterium or even a small collection of disease-protective bacteria will facilitate determining the mechanism of action—from the perspective of both the host and the bacterium—to better understand which specific patient populations will benefit from the treatment.”
Reaching such levels of precision, though, will probably depend on teamwork. “Although the first decade of microbiome research really focused on associations between the microbiome and various disease states, there is beginning to be a greater appreciation that mechanistic, causal studies need to be performed to more effectively translate these findings to the clinic,” Surana said. “Unfortunately, every step of this process represents a challenge, each of which requires unique skill sets: bioinformatic identification of microbes that are likely causally related to disease protection, isolating and culturing the identified bacteria, and testing the effects of these microbes in relevant animal models.”
A variety of improvements in technology could smooth the pathway to higher accuracy in microbiome-based treatments. “Ultimately, these efforts often require collaborative work between multiple groups, each with expertise in each of these different areas.” Much like microbes work together, scientists will need to do the same to turn these microorganisms into medicine.
References
1. Surana, N.J., Kasper, D.L. Moving beyond microbiome-wide associations to causal microbe identification. Nature. 552(7684):244–247. (2017).
2. Sepich-Poore, G.D., Zitvogel, L., Straussman, R. et al. The microbiome and human cancer. Science. 371(6536), eabc4552. (2021).
3. Davar, D., Dzutsev, A.K., McCulloh, J.A., et al. Fecal microbiota transplant overcomes resistance to anti–PD-1 therapy in melanoma patients. Science. 371(6529):595–602. (2021).
4. Baruch, E.N., Youngster, I., Ben-Betzale, G. et al. Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science. 371(6529):602–609. (2021).
5. Gopalakrishnan, V., Spencer, N., Nezi, L. et al. Gut microbiome modulates response to anti–PD-1 immunotherapy in melanoma patients. Science. 359 (6371):97–103. (2018).
6. Blacher, E. Can microbes combat neurodegeneration? Science. 373(6551):172–173. (2021).













