A new study has produced a proof of principle for a new “universal” means of treating COVID-19. Using messenger RNA packaged in lipid nanoparticles, scientists showed in a mouse model that host cells can produce a “decoy” enzyme that binds to coronavirus spike proteins, meaning the virus shouldn’t be able to latch onto cells in the host’s airway and start the infection process.
“Rather than messenger RNA as a vaccine, this shows that mRNA can be used as a universal therapy against different coronaviruses,” said Gaurav Sahay of Oregon State University (OSU) and senior author. “Despite mass vaccination, there is an urgent need to develop effective treatment options to end this pandemic. Several therapies have shown some effectiveness, but the virus’ high mutation rate complicates the development of drugs that treat all variants of concern.”
The group’s most recent findings were published in Advanced Science.
Next steps involve showing that the protein prevents infection in mice, said Sahay, who added that the mRNA treatment is possibly “a couple of years” away from being available to human patients.
In their study, Sahay and collaborators showed that, in a mouse model, it’s possible to prompt production of a protein that can block multiple variants of the SARS-CoV-2 virus from entering cells and causing respiratory disease.
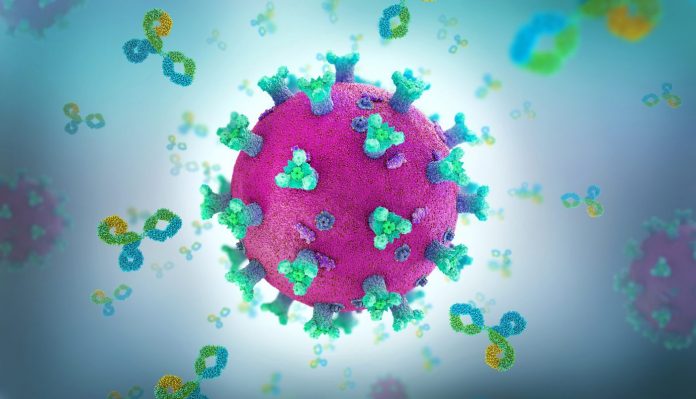
Breathing in the virus is the primary way to contract COVID-19, blamed for 6 million deaths globally since the pandemic began in late 2019. The virus’ envelope is covered in spike proteins that bind to an enzyme produced by cells in the lungs.
The study involved messenger RNA that was administered intravenously and also through inhalation, which would be the preferred delivery method for humans.
HACE2—short for human angiotensin-converting enzyme 2—is an enzyme of the airway cells. It is also expressed in the heart, kidney and intestine, and has a hand in numerous physiological functions.
Simply giving a COVID-19 patient hACE2 would have limited effectiveness in treating the disease, Sahay said, because the soluble form of the enzyme, the kind that can circulate throughout the body, has a short half-life—less than two hours, meaning it wouldn’t stay in a person’s system very long.
But lipid nanoparticles (LNPs), containing mRNA that orders production of the enzyme, can overcome that problem.
In this study, the researchers engineered synthetic mRNA to encode a soluble form of the enzyme, packaged the mRNA into lipid nanoparticles and delivered it to cells in the liver with an IV; within two hours, the enzyme was in the mice’s bloodstream, and it stayed there for days.
The scientists also delivered the loaded LNP via inhalation, prompting epithelial cells in the lungs to secrete soluble hACE2.
“The soluble enzyme effectively inhibited live SARS-CoV-2 from infecting host cells,” said OSU postdoctoral researcher Jeonghwan Kim. “The synthesis of mRNA is fast, affordable and scalable, and LNP-delivered mRNA can be repeated as necessary to sustain protein production until the infection subsides. Once treatment stops, the no-longer-needed soluble hACE2 clears the system in a matter of days.”













