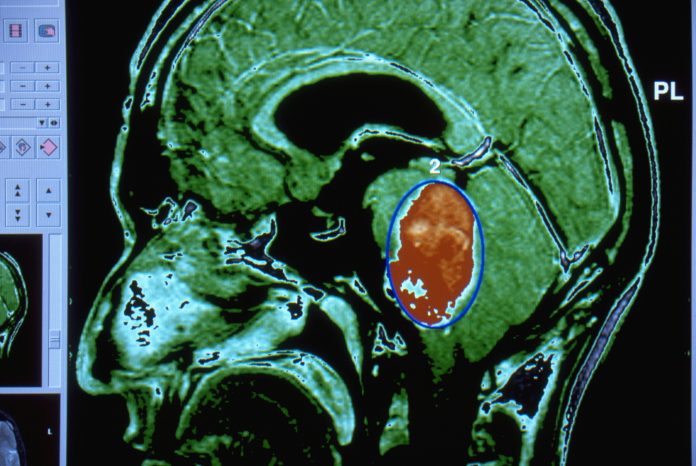
Medulloblastoma (MB) is the most common malignant pediatric brain tumor, accounting for 20% to 25% of all childhood brain cancers, but with few effective treatments for high-risk medulloblastoma types. But a new way of mapping medulloblastoma genes has led researchers to a novel type of cancer therapy that appears to be an effective treatment for the most aggressive form of the disease.
Using a network-based systems-pharmacogenomics approach, a team led by researchers from The University of Queensland’s (UQ) Diamantina Institute and the The Walter and Eliza Hall Medical Institute (Institute) WEHI in Melbourne sought to find new candidate drugs for MB. The technique is built on a functional genomics screen that identified a network of protein-protein interactions implicated in promoting aggressive medulloblastoma. From that information, the researchers were able to pair drugs with a particular mechanism of action to gene expression data derived from medulloblastoma patients. The final drug-target network contained 145 proteins and 36 drugs.
There are four general medulloblastoma types: Wingless (WNT), Sonic Hedgehog (SHH), Group 3, and Group 4. The non-WNT subtypes are the most aggressive. After five years of study, four gene drug targets – CDK4, CDK6 and AURKA – and the drugs that target them were revealed as strong candidates for MB. For aggressive, non-WNT medulloblastoma, the team focused on novel drugs targeting TUBB, CAD, SNRPA, SLC1A5, PTPRS, P4HB and CHEK2. TUBB emerged as a leading candidate from their network analysis.
“These are drugs already approved for other diseases or cancers but have never been tested in pediatric brain tumors,” said UQ lead researcher Laura Genovesi.
The team homed in on ixabepilone, typically used to treat breast cancer, on the idea it would block tumor growth. Ixabepilone is an Epothilone B agent, one of a class of a new generation microtubule-stabilizing agents (MSA) that bind to the β-tubulin subunit of microtubules. Of the three Epothilone B agents, patupilone, ixabepilone and sagupilone, ixabepilone is the most mature analogue in development.
In preclinical models, ixabepilone halted tumor growth and extended the survival rate in mice bearing patient-derived xenograft tumors of the Sonic Hedgehog and Group 3 subtype providing the first demonstration of its efficacy in medulloblastoma.
“Targeting TUBB via ixabepilone in four PDX models confirms this new generation MSA as an effective therapy for aggressive MB and validates an additional target from our functional network, demonstrating its power for the discovery of new MB therapies through drug repositioning,” the authors write.
Ixabepilone is the second drug the team has identified using their genetic mapping screen that has shown a high degree of efficacy against medulloblastoma.
Associate Professor Melissa Davis, joint senior author from WEHI, said the chemotherapy drug had a ‘dramatic survival benefit’, with very little sign of any remaining tumor following treatment.
“The impact of this drug in our model systems gives hope for children diagnosed with highly aggressive forms of medulloblastoma,” said Melissa Davis, joint senior author from WEHI. “But even more promising, is the potential to use our genetic map to find other treatments for this disease. We now have an entire list of proteins and pathways that new therapeutics could target that we know would kill cancer cells.”











