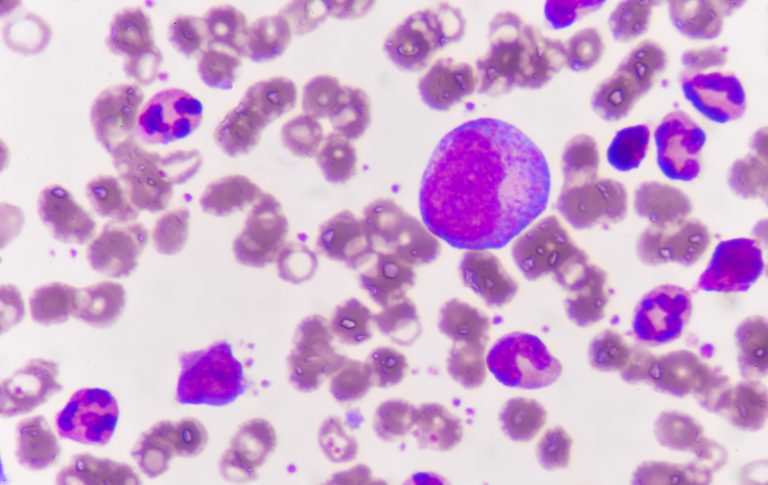
Scientists at St. Jude Children’s Research Hospital have discovered a mutation in pediatric acute myeloid leukemia (AML) that physicians can use to identify patients with a high-risk of relapse. A paper on the work was published in Blood Cancer Discovery, a journal of the American Association for Cancer Research.
“We were very much interested in understanding relapsed disease in AML,” says said co-corresponding author Jeffery Klco, MD, PhD, St. Jude Department of Pathology whose laboratory focuses on understanding the mechanisms and genomics of AML. From a large cohort of relapsed pediatric AML samples at the hospital, Klco and colleagues sought to identify which mutations were enriched in relapsed disease and better understand why some children relapsed and others did not.
A complex high-risk subtype
It became clear early on that there were a couple of cases who had alterations in the gene UBTF. As they dug in, they realized that the complexity of the mutation was masking its detection.
After revamping their study pipeline, Klco’s team and colleagues evaluated the genomics of 136 St. Jude patients treated for relapsed AML. Their study revealed a UBTF exon 13 tandem duplication (UBTF-TD), which was present in nearly 10% of relapsed pediatric AML. “We feel this is a new entity of pediatric AML,” says Klco.
“First, we needed to adjust the computational pipeline to discover fusions and indels,” says Klco. The first pipeline could detect some but not all of them in these patients. While researchers have been sequencing relapsed AML samples over the years the UBTF-TD mutation could not often be found. “This explains why lots of studied missed finding this mutation over the years,” he says. “We discovered it is much more common than people originally thought,” Klco explains. After reviewing the cohort from TARGET AML study, the largest study of pediatric AML at diagnosis, the team discovered a large number that were missed.
UBTF-TD AML is more common in children than adults. “About 4% of children with AML have this mutation at diagnosis,” says Klco, adding the mutation is not found in AML cases with other driver alterations.
Poorer outcomes
When the team extended their research to other cohorts for outcomes study it became clear that UBTF-TD AML is also associated with poor outcomes and an increased incidence of minimal residual disease (MRD). MRD refers to cancer cells that persist in small numbers after initial treatment, often giving rise to recurrence of the cancer.
“One of the strongest associations was with FLT3-ITD status, suggesting that many of the poor outcomes ascribed with FLT3 mutations are probably related to UBTF tandem duplications,” adds Klco. FLT3-ITD mutations are among the most common mutations in pediatric AML.
Bone marrow transplant trajectory
Looking for the presence of this mutation at diagnosis could help identify those patients at high-risk for relapse. “I expect this will rapidly become one of the high-risk molecular features of pediatric AML,” says Klco. “If a patient is unfortunately diagnosed with a UBTF-TD, it puts them on a different trajectory and push them more towards more aggressive treatment upfront, including bone marrow transplant.”