A new, updated risk score can help predict contrast-associated acute kidney injury (CA-AKI) among patients undergoing percutaneous coronary intervention (PCI), Mount Sinai researchers report. According to their study, the tool can enhance management of patients at high risk of CA-AKI before, during, and after PCI, and improve prognosis following the procedure.
The risk score, called “The Mehran-2 CA-AKI Risk Score,” was developed by Roxana Mehran, MD, Professor of Medicine and Population Health Science and Policy, and Director of Interventional Cardiovascular Research and Clinical Trials at the Icahn School of Medicine at Mount Sinai, along with other Mount Sinai cardiologists. Their results were presented today at the American Heart Association Scientific Sessions 2021, and simultaneously published in The Lancet.
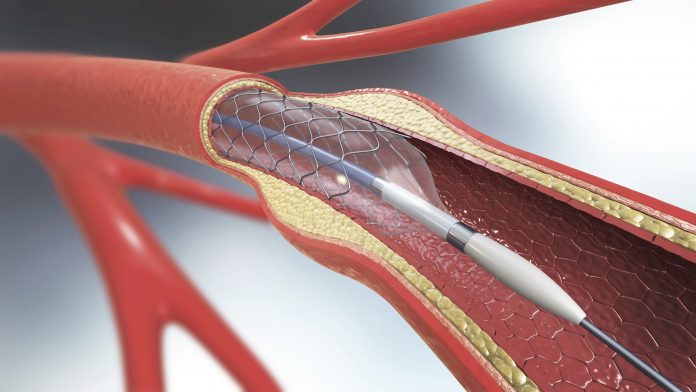
Patients with coronary artery disease often undergo PCI, in which interventional cardiologists use a catheter to place stents in the blocked coronary arteries to restore blood flow. Cardiologists use angiography to determine which arteries have the most severe blockages, and inject iodinated contrast into the bloodstream. That fluid is toxic, and high-risk groups can have kidney problems as a result.
“Although the incidence of CA-AKI has decreased over the past few years, it remains a significant complication of PCI and is associated with mortality, prolonged hospital stay, and increased medical costs,” explains Mehran. “Simple measures can be taken around the time of procedure when a patient is identified to be at high risk of CA-AKI, and we hope this new score is widely adopted to enhance the care of patients and improve outcomes.”
Mehran’s new risk score expands upon her initial risk score developed in 2004 that was widely implemented in cardiac catheterization labs around the world. The updates take into account changes in practice surrounding PCI, including more advanced imaging techniques that require less toxic contrast agents, as well as improved stents.
To update the risk score, researchers looked at records of 30,000 patients who underwent PCI at The Mount Sinai Hospital from 2012 to 2020. All patients had documented creatinine tests—measuring how well kidneys are working and filtering waste from the blood—both pre procedure and 48 hours post procedure, as well as a one-year follow-up.
Mehran and her team created a predictor model identifying which patients are at highest risk of acute kidney injury based on baseline risk factors, which included diabetes, anemia, congestive heart failure, advanced kidney disease, acute heart attack, and ST-segment elevation myocardial infarction (STEMI), or complete blockage of a major heart artery. Being older than 75 was also considered a risk factor. They assigned an individual score to each of those risk factors, then calculated patients’ overall risk score, putting them in specific groups: between 0-4 was “low risk,” 5-9 was “moderate risk,” 10-13 was “high risk,” and anything above 14 was “extremely high risk.”
By calculating patients’ risk score and figuring out what risk category they fit into, doctors can modify their periprocedural management approach to improve outcomes. This may include increasing hydration before PCI, administering statins, and minimizing the amount of contrast used during the procedure.
“Acute kidney injury after invasive procedures remains a mystery since it has such a robust adverse prognosis, yet we still don’t know of a clear responsible mechanism. Therefore, it remains a very challenging and interesting research field,” explains senior author George Dangas, MD, PhD, Professor of Medicine (Cardiology) and Director of Cardiovascular Innovation at the Zena and Michael A. Wiener Cardiovascular Institute at Icahn Mount Sinai.













