Two patient-driven cancer organizations focused on lung cancer and Champions Oncology, a research and development company that leverages patient-derived xenograft (PDX) studies to inform clinical development, have launched a new research initiative aimed at developing a better understanding of the unique characteristics of epidermal growth factor receptor (EGFR) positive lung cancer.
The new study was conceived by patient-centric organization the Addario Lung Cancer Foundation (ALCF) and the EGFR Resisters which has established a collaboration between the Addario Lung Cancer Medical Institute (ALCMI), and a leading researcher in EGFR mutant lung cancer, Pasi A. Jänne, M.D., Ph.D., of Dana-Farber Cancer Institute.
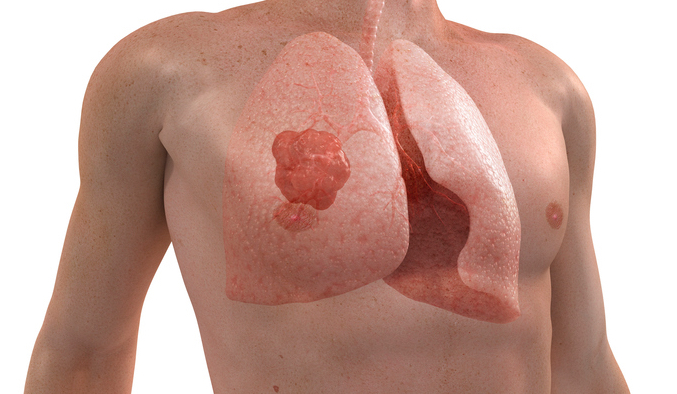
The ALCMI-012 study, A Prospective Biospecimen Collection Study from Patients with EGFR mutant Tumors, will collect a small amount of tumor or pleural fluid from patients who require biopsies or surgery and have agreed to donate a portion of their tumor. Champions Oncology will use these samples to create models of these tumors in mice with limited immune function. Champions will then make the mouse models available to researchers worldwide to help foster and broader EGRF mutant research aimed at better understanding why some patients with EGFR positive lung cancer develop resistance to treatment.
“As a lung cancer patient and a friend of many other lung cancer patients and their families, I know firsthand how heartbreaking it is to develop resistance to treatment,” said Teri Kennedy, an EGFR-positive lung cancer patient and one of the founders of EGFR Resisters, in a press release. “This grassroots, patient-driven community hopes to empower patients to participate to find cures and work with researchers to advance research.”
The study is currently open to patients in the U.S. and Canada and does not require patients to travel outside their local area to participate. ALCMI’s research team will work directly with patients and their treating physicians to collect tissue and fluid specimens.
“This study provides an opportunity to change EGFR positive lung cancer into a manageable, chronic disease,” said Jänne, who is the lead investigator of the research. “It's my hope that every patient diagnosed with a resistant EGFR mutation will take part and help speed the progress toward lasting treatments.”
According to the National Cancer Institute, more than 60 percent of non-small cell lung carcinomas (NSCLC) express EGFR, making it a fertile target for NSCLC treatment. Treatment of the disease today most often focuses on the use of tyrosine kinase inhibitors (TKIs), which have been shown to be especially effective in patients whose tumors harbor activating mutations in the tyrosine kinase domain of the EGFR gene.
But there are many variations of EGFR mutations that have implications on treatment. EGFR patients with specific genetic markers (L858R, T790M, exon 19 deletion) respond well to targeted therapies initially, but later develop resistance to treatment. Further, there is no known treatment for patients with an exon 20 deletion, a very rare EGFR mutation. The overarching goal for the study is to better understand the mechanisms of resistance to therapy for EGFR positive patients and to eventually develop new, more effective treatments.











