Researchers at the University of Pittsburgh have developed a universal receptor system that allows T cells to recognize any cell surface target, providing the possibility for tailored CAR T cell and other immunotherapies used to treat diseases such as cancer.
T cell therapies, especially those involving CAR T cells are becoming increasingly popular as cancer and autoimmune disease treatments, with several CAR T cell therapies having shown impressive results in clinical trials and being approved by the FDA.
For this type of immunotherapy, a patient’s own immune cells are genetically engineered to express chimeric antigen receptors (CAR) that will normally target one protein expressed on the diseased cells specifically. While the technology has proven efficient, if the targeted cells evolve to lose the protein of interest, the T cells have to be re-engineered resulting in an expensive and time-consuming process.
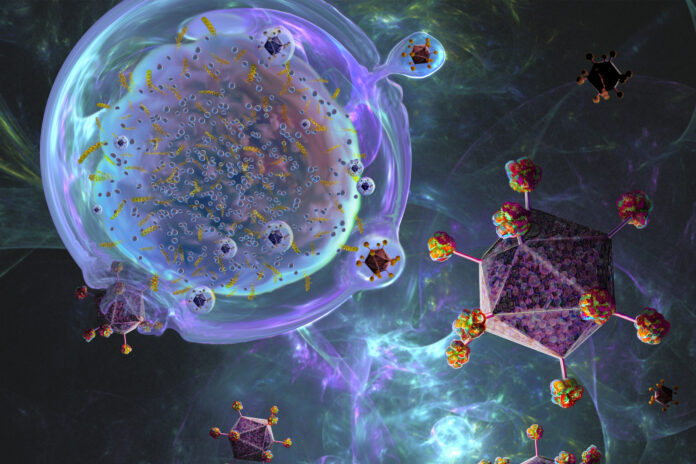
Reporting in Nature Communications, scientists have now developed T cells with receptors containing a universal “SNAPtag” which allows them to bind to antibodies targeting different proteins. The tag consists of an enzyme which can form covalent bonds with an antibody carrying a specific molecule called benzylguanine. By modifying the antibody dosage, treatments could be adjusted to provide the optimal immune response.
In their study, the researchers were able to show that their SNAP technology works for the previously mentioned CAR T cell receptors as well as SynNotch receptors which can be used to activate a series of genes.
“We showed for the first time that we can make a universal SynNotch receptor. This SNAP-SynNotch system is super programmable because you can have both designer input and designer gene output,” said Jason Lohmueller, PhD, assistant professor of surgery and immunology in the division of surgical oncology at the Pitt School of Medicine and senior author of the study.
“Our hope is that we can use this approach to make cell therapies and deliver genes for cancer, autoimmune disorders, organ transplantation tolerance and more.”
The “SNAPtag” modified T cells are administered together with the cancer-targeting antibodies labeled with benzylguanine. Via a reaction known as bioorthogonal chemistry, which occurs in living systems without disturbing natural processes, the SNAPtag fuses the antibody to the receptor.
“What’s unique about our approach is how the T cell interacts with the antibody. It’s not just binding, but fusingvia covalent attachment—the strongest form of chemical bond,” explained Lohmueller.
The scientists used human tumor xenograft mouse models for their research, showing that treatment with SNAP-CAR T cells significantly decreased the size of tumors and prolonged survival of the animals. According to the researchers, this important proof-of-concept will be further expanded to be used in clinical trials with Coeptis Therapeutics which have licensed the technology from the University of Pittsburgh.