The Translational Genomics Research Institute (TGen), an affiliate of City of Hope, in association with HonorHealth Research and Innovation Institute and Systems Biology Ireland (SBI), have begun a clinical trial, testing the combination of two drugs against advanced pancreatic cancer, one of the most deadly and difficult-to-treat malignancies.
The trial combines two drugs — Vemurafenib and Sorafenib — to treat advanced pancreatic cancer in patients whose cancer has spread following conventional chemotherapy.
The trial is named for Dr. Nate Nieto, a Northern Arizona University (NAU) microbiologist known for his insights into infectious diseases and wildlife ecology. He was a frequent collaborator with TGen on infectious-disease investigations, including those involving hantavirus and Lyme disease. Dr. Nieto succumbed to advanced pancreatic cancer in 2019 at age 44, at the height of his research career.
In the wake of his illness, Dr. Nieto’s friends came together and used their expertise in systems biology, mathematics and computational biology to find a new way to target pancreatic cancer. Their efforts identified Vemurafenib and Sorafenib as a drug combination that would target the KRAS gene, and resulted in a new mathematical modelling system to predict the effectiveness of this drug combination. KRAS mutations act as molecular on/off switches for this disease, and are believed responsible for up to 90% of pancreatic cancers.
Dr. Nieto’s inspiration drives researchers
“Nate’s colleagues, caregivers and friends, some of whom are involved in this treatment study, have come together to test this systems-based approach in the treatment of pancreatic cancer,” said Daniel D. Von Hoff, M.D., TGen Distinguished Professor, consulting investigator on the clinical trial, and one of the nation’s leading authorities on pancreatic cancer.
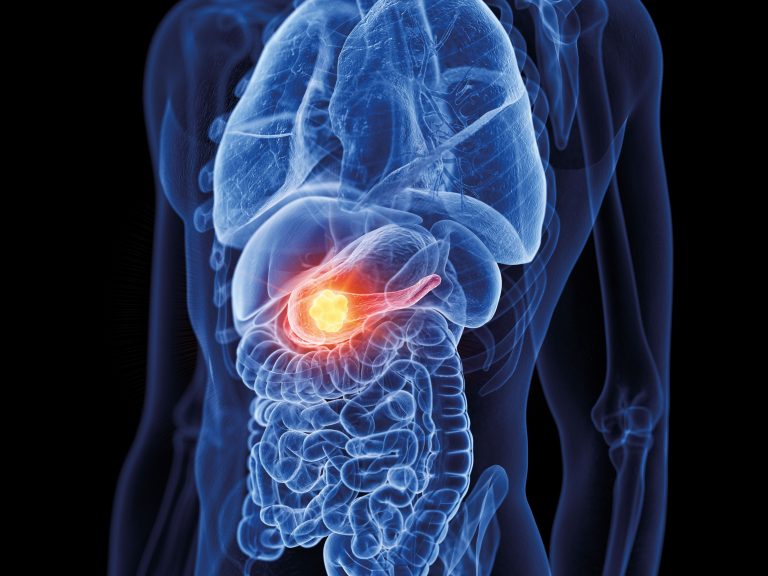
Pancreatic cancer is the third-leading cause of cancer death in the U.S., annually killing nearly 50,000 Americans. It usually is not detected within the abdomen until its advanced stages, when it is more difficult to treat, resulting in a patient 5-year survival rate of only about 9%.
“Additional treatment strategies are desperately needed to improve long-term survival in these patients,” said Erkut Borazanci, M.D., a medical oncologist and physician-investigator at HonorHealth, a clinical associate professor at TGen, and this clinical trial’s principal investigator. “We hope that we can target the KRAS mutation that is most common in pancreatic cancer with this combination.”
The mathematical model was perfected by SBI at the University of Dublin in association with NAU and the Los Alamos National Laboratory. It predicts how cancer-causing RAS cell-signaling can be efficiently blocked by RAF proteins.
Potential application in other cancers
“This is the first clinical trial I’m aware of that is based on a mathematical model of signal processing,” said Professor Walter Kolch, Director of SBI. “It is a big step towards SBI’s big vision of building ‘digital twins’ of patients that allow us to test treatments in silico (computer models) and select the best one before we give them to patients.”
If proven successful against pancreatic cancer, this clinical trial could lead to extensive applications in other RAS-mutant cancers, such as colorectal and lung cancers.
Besides testing the safety and effectiveness of Vemurafenib combined with Sorafenib, the study is intended to advance the use of “liquid biopsy” blood tests — examining short segments of ctDNA shed from the cancer into the blood circulatory system — to identify different types of mutations and measure the amount of ctDNA coming off the tumor. This process was pioneered by TGen.
Vemurafenib, made by Roche, has already received U.S. Food and Drug Administration (FDA) approval for the treatment of patients with melanoma. Sorafenib, made by Bayer, is already FDA-approved for the treatment of patients with liver, kidney and thyroid cancers. Pre-clinical laboratory studies have demonstrated a “synergistic effect” of combining the two drugs.
Over the course of a year, the clinical trial will involve about 10 patients who specifically have pancreatic ductal adenocarcinoma (PDAC), and have G12D mutations in the KRAS gene.













