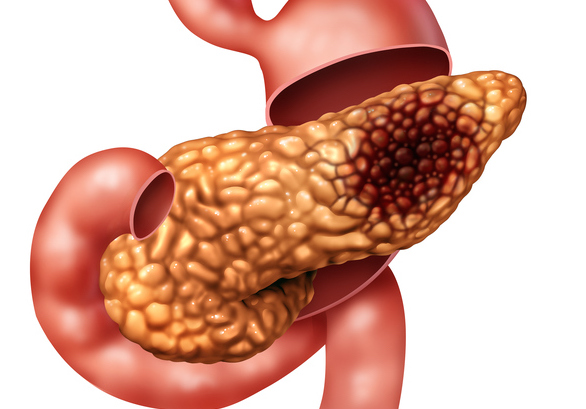
A new study that analyzed the tumor microenvironment of pancreatic ductal adenocarcinoma (PDAC) revealed new insights into why immunotherapy does not work well in this cancer type. The researchers identified new targets and potentially new treatments focused on providing successful immunotherapy-based strategies.
This study, led by researchers at the Johns Hopkins Kimmel Cancer Center, is the latest from an ongoing platform trial formed in 2015 to study immunotherapy treatments before surgery (neoadjuvant) and after surgery (adjuvant) in patients with pancreatic cancer.
“We started the platform trial to better dissect the tumor microenvironment of a pancreatic tumor, to see what factors inhibited the cancer’s response to immunotherapy, “explained study co-leader Lei Zheng, MD, PhD, co-director of the Pancreatic Cancer Precision Medicine Center of Excellence Program and professor of oncology at Johns Hopkins. By giving immunotherapy two weeks prior to surgery, and then retrieving a large amount of tissue during surgery, researchers have access to the whole tumor, not just a small amount such as contained in a biopsy.
In this portion of the study, the team used those banked biospecimens and studied the tissue, cellular and molecular structure of the tumor microenvironment by employing multiomic strategies, meaning they explored the genetic alterations (DNA), transcriptomes (RNA) and proteins expressed. Their results are published in Cancer Cell.
The team first tested two proven treatment strategies known to stimulate T-cells, the essential component of immunotherapy. One is GVAX, a therapeutic vaccine that can stimulate the patient’s immune system to attack the cancer. The other is anti-PD1 antibody immunotherapy with nivolumab, which is already standard of care for some cancers. However, neither is effective in pancreatic cancer.
Combining the two approaches were still insufficient for pancreatic cancer. “But we gained some important insights into the reasons why,” said Zheng.
To be effective, T cells need to get into the pancreatic tumor. While the vaccine did that job, those T-cells were quickly exhausted, losing their ability to mount a sustained immune response. Adding the anti-PD1 antibody helped those T cells be more functional. “But what becomes more functional is not the CD8 T cell, it is the CD4 T cell,” says Zheng. The CD4 T cells are regulatory T cells that act on CD8 T cells, or effector T cells. And the CD8 T cell is the cell that can kill cancer cells.
“So what we discovered is that the combination creates a better regulatory site to make more functional CD8 cells,” explained Zhang. But the team learned they were still missing an important signal because the combination did not produce enough effector T cells and that the T cells were not sufficiently activated.
According to Zheng, that missing signal is CD137. “We found that if patients have CD137 on their T cells they live longer,” he said. “You need to activate CD137 in order to make those T-cells more active and for their activity to be sustained.”
Their research also revealed that neutrophils—created by immune cells to fight infection—are hijacked by pancreatic cancer cells to suppress T cell activation.
As a result of these findings, the researchers began testing two new treatment strategies: anti-CD137 agonist antibody treatment in combination with anti-PD-1 immunotherapy to activate T cells, and anti-IL-8 neutrophil-blocking antibody treatment in combination with anti-PD-1 immunotherapy to prevent the inactivation of T cells.
“By adding the CD137 agonist antibody, it provided meaningful improvement, as did the anti-neutrophil treatments,” said Zheng, adding that he hopes these new insights may improve survival after surgery in pancreatic cancer.













