Under normal circumstances, pancreatic tissue is considered microbe-free. But a new study found that pancreatic cancer tumors harbor a large microbiome, its presence impacts cellular function, and is associated with poorer patient outcomes. The findings, published in Cancer Cell, provide evidence that the pancreatic tumor microbiome reflects or influences the trajectory of pancreatic tumor growth.
“In our study, the pancreatic cancer samples had a lot of microbes and we found that they were impacting the cellular metabolism, DNA damage, as well as inflammation, which were impacting both the functions of the cells, but also how they were interacting with other cells in the microenvironment,” said Subhajyoti De, PhD, principal investigator at Rutgers Cancer Institute and senior author of the study. By comparison, healthy pancreatic tissue had very little microbial presence.
De mentioned two long-standing issues: why does pancreatic cancer have such a bad survival rate and why doesn’t immunotherapy work for this tumor type. “Our study suggests that a lot of the immune cells within the pancreatic cancer microenvironment might actually be fighting against the infection and not fighting against the tumor and that’s why the immunotherapy is not that effective,” he said. “It might just be that maybe the microbes are driving the immune cells away from the cancer fight.”
The team relied on a new genomic approach to help distinguish the source of microorganisms within the tumor environment. They developed a technique called SAHMI (Single-cell analysis of Host-Microbiome Interactions) to identify microorganisms associated with individual human cells.
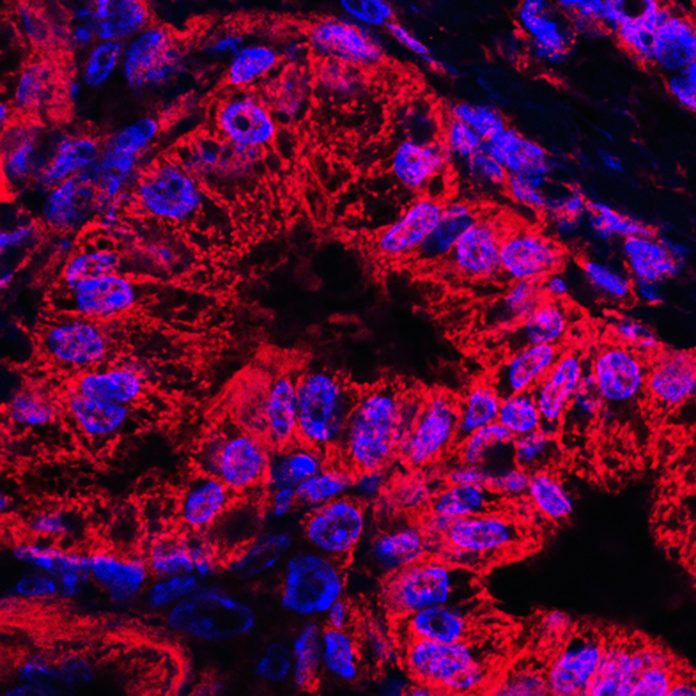
“We took the pancreatic tumor tissue and created single cell suspensions followed by sequencing of the individual cells and contents within the cells,” explains De. “When we studied millions of RNA sequences from the individual cells with SAHMI, we could discern between human RNA and other species and could find out which microbes were in the tumor.”
Studying two independent groups of pancreatic tumors, the team found that some had bacteria that associated with specific cell-types within the tumor, which were essentially absent in normal pancreatic tissues. These bacteria were predominantly located within tumor cells, and their abundance correlated with cancer-related cell activities. The specific signatures of the microbes that were found predicted particularly aggressive cancer progression and poor prognosis. “This new technique allowed us to identify tumor-associated microbes and measure the activity of the host cells at the same time,” added De.
The microbial footprints within the pancreatic tumors raised the question of whether the immune cells that were present were responding to the cancer or to the microbes. “We do not know that for sure, but it might be a combination of them both,” said De. “We do know that most types of cancer, including those that we thought historically are not associated with microbes, do in fact, have microbes.” He theorizes that in some cases, the microorganisms might be bystanders, just exploiting the free resources available. “In other cases, they might be impacting both the immune response and also the DNA damage or anything else that might be happening within the tumor,” he added.
Looking ahead, De and colleague plan to learn more about how the microbes are impacting cellular functions—which microbes might be good, which microbes might be bad. And in terms of possible clinical studies, they would like to see whether the microbial infections have any impact on the response to the treatment, particularly immunotherapy. Said De, “Perhaps this will then give us some indication why immunotherapy might not be effective so we can re-engineer some aspects of it to improve it.”













