People with specific autoantibodies in their blood on admission to hospital with COVID-19 are more likely to progress to severe disease, according to research led by New York University Grossman School of Medicine.
These autoantibodies, which attack components of the blood rather than protecting against disease, were found in more than 30% of individuals on admission to hospital and their presence was a significant predictor of a negative prognosis.
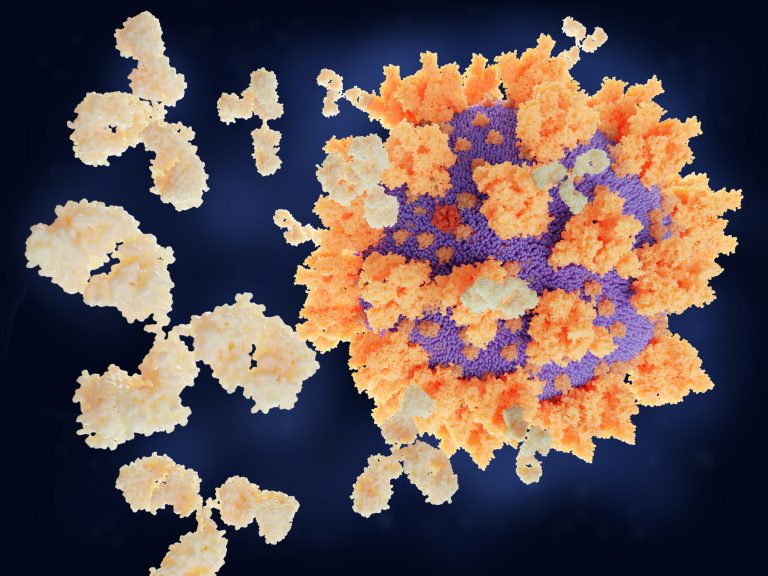
Unlike normal antibodies, which are developed to help to fight off future infections, autoantibodies can cause harm to the body by triggering an attack on its own cells or tissues. For example, they are common in the early stages of many autoimmune conditions such as rheumatoid arthritis and type 1 diabetes.
“Although autoantibodies have been observed in different viral and nonviral infections, the high percentage of COVID-19 patients with autoantibodies… indicates that the levels of autoreactivity are particularly high in this infection,” write the researchers in the journal Life Science Alliance.
Ana Rodriguez, a professor at New York University, and colleagues investigated whether the high levels of autoantibodies observed in COVID-19 patients could be linked to disease severity.
They analyzed samples from 115 patients hospitalized with SARS-CoV-2 infection and 42 uninfected controls and assessed the levels of autoantibodies against red blood cell lysate, the lipid phosphatidylserine and DNA. The team chose these autoantibodies as they have previously been shown to be high in patients with autoimmune diseases such as lupus and also infectious diseases such as malaria.
The patients in the cohort had a range of different ethnic backgrounds (White, Black, Asian, and Hispanic) and were hospitalized with COVID-19 at NYU Langone hospitals between April and June 2020. Up to 36% of the individuals in the study had IgG autoantibodies against red blood cell lysate. Patients with autoantibodies against phosphatidylserine and DNA on admission to hospital were significantly more likely, 93% and 86%, respectively, to progress to having more severe disease, such as needing a ventilator, than those that did not.
Overall, 24% of individuals in the group that progressed to having severe COVID-19 had autoantibodies against either DNA or phosphatidylserine.
“While further testing is needed, our findings suggest that a test for the presence of anti-DNA and anti-phosphatidylserine antibodies could help identify those COVID-19 patients admitted to hospital who are most at risk of needing intensive care and who need to be monitored more closely,” said Marisol Zuniga, a researcher at New York University and study author, in a press statement.
These results agree with earlier observations of patients with severe COVID-19 infection where an excessive immune reaction accounts for much of the cell and tissue damage caused by the infection.
“These observations suggest that the most severe forms of disease observed in COVID-19 patients may be a result of the host response to infection, rather than a direct consequence of viral cytopathic effect,” write the authors.
“Autoantibodies, as part of the host response to infection, may contribute to this delayed pathogenesis through different mechanisms. Our work suggests that anti-DNA and anti- phosphatidylserine antibodies may have a role in different pathogenic processes, including cell injury and coagulation, constituting a possible mechanism contributing to pathogenesis in COVID-19 patients.”













