Scientists Cedars-Sinai Medical Center have discovered that some types of highly aggressive soft-tissue sarcoma tumors create high levels of the protein macrophage migration inhibitory factor (MIF), a protein that normally blocks tumor growth. But instead of blocking cancer, MIF does the opposite in these sarcomas, ultimately leading to tumor growth. A study describing the discovery, led by researchers at Cedar-Sinai Cancer Center, was published in Cell Reports.
Soft-tissue sarcoma is a rare type of cancer that forms in the muscle, fat, blood vessels, nerves, tendons, and joint lining. It most commonly occurs in the arms, legs, and abdomen, and kills more than 5,000 people in the U.S. each year, according to the American Cancer Society. Unfortunately, the standard of care for treating these recurrent and aggressive soft-tissue sarcomas is largely unsuccessful.
“Targeting components of the tumor microenvironment have shown promise for many solid tumors yet have been only marginally assessed for sarcoma, partly because knowledge of the sarcoma microenvironment composition is limited,” the authors wrote.
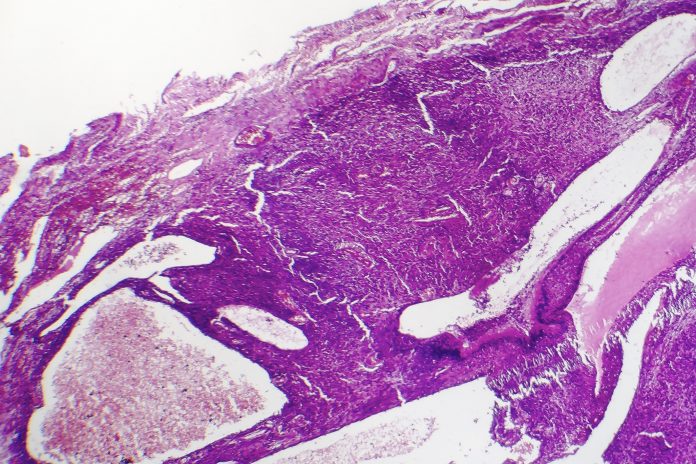
To learn more about the microenvironment of these cancers, the researchers studied a variety of soft-tissue sarcoma samples in humans and laboratory mice. They noted that these tumors present with a high level of myeloid cells, cells that normally function to detect pathogens and initiate an immune response.
“It was striking that such a large percentage of the immune cells were myeloid cells, and we thought that since they obviously weren’t killing the tumor cells, they must be doing something to promote tumor growth,” said Stephen Shiao, MD, PhD, division director of the Division of Radiation Biology, co-leader of the Translational Oncology Program and a co-author of the study. “And indeed, our analysis of tumor samples showed that many of the myeloid cells had adopted a tumor-promoting function.”
Myeloid cells are the most abundant immune components of sarcomas as well as many epithelial tumors, in which they become tumor-associated macrophages (TAMs). “While in principle, macrophages could have anti-tumorigenic properties, the tumor microenvironment critically re-shapes the activities of TAMs such that they positively contribute to tumor growth,” the authors wrote, by creating an immunosuppressive microenvironment, favoring angiogenesis and by releasing metabolites that have recently emerged as drivers of drug-resistance.
To learn more, the researchers conducted comprehensive single-cell RNA sequencing characterization of sarcoma-associated macrophages and their expression programs, including the mechanisms of interaction with the tumor cells.
When assessing the proteins excreted by the cancer and the myeloid cell receptors, they found that the MIF pathway was highly upregulated in certain types of macrophages found in the sarcoma tumor. Other studies, including the Cancer Genome Atlas, have shown that cancers with elevated MIF are associated with poorer prognoses but have not discovered a mechanism for this.
“Sarcoma cells use MIF to interact with macrophages expressing the CD74 receptor on myeloid cells to switch their activation state to a pro-tumorigenic potential,” the authors wrote. In short, the myeloid cells had receptors to sense the MIF proteins making them switch their biology and promote, rather than block, tumor growth.
When the investigators generated tumors from cancer cells that didn’t express MIF, the tumors were smaller and myeloid cells were able to penetrate the tumors and check tumor growth. They team observed that blocking MIF expression favored the accumulation of macrophages with inflammatory and antigen-presenting profiles. The authors speculate that either the myeloid cells attacked the tumors directly or might have activated other immune cells to do so.
“This work identifies the MIF/CD74 axis as a critical determinant of tumor microenvironment composition in sarcoma,” the authors noted, suggesting this information could be used to create novel therapies that re-shape the sarcoma microenvironment. They suggest that a medication designed to stop cancer cells from expressing MIF could be evaluated in combination with existing therapies to see if it improves outcomes.
“The majority of studies in cancer biology and immunotherapy have been done on carcinoma, the most common type of cancer,” said senior author Jlenia Guarnerio, PhD. “Much work has been done to describe which types of immune cells infiltrate these tumors and how carcinoma cells interact with immune cells, but there is almost no research on sarcomas. We need to continue our investigation so that we understand the roles of many other cells—T cells and B cells, for example—and how all the players work together.”
The team is now working in the lab and with outside partners to develop MIF-targeted compounds.











