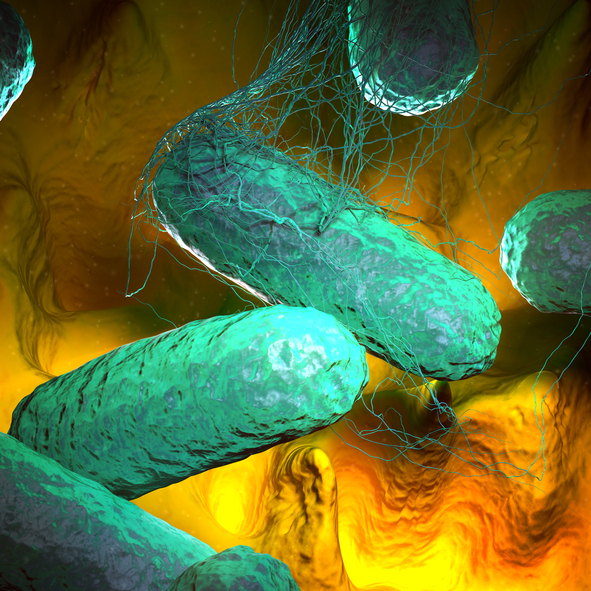
Research led by Stanford University shows that Salmonella enterica serovar Typhi (S. Typhi), the bacteria responsible for causing typhoid fever, is mutating and becoming increasingly resistant to antibiotics and these resistant strains are spreading quickly.
Jason Andrews, an associate professor at Stanford University, and colleagues found almost all the resistant strains originated in South Asia and have spread to other countries at least 200 times since 1990.
“The speed at which highly-resistant strains of S. Typhi have emerged and spread in recent years is a real cause for concern, and highlights the need to urgently expand prevention measures, particularly in countries at greatest risk,” commented Andrews in a press statement.
“At the same time, the fact resistant strains of S. Typhi have spread internationally so many times also underscores the need to view typhoid control, and antibiotic resistance more generally, as a global rather than local problem.”
Despite the existence of vaccines against typhoid fever and antibiotics to treat the condition (ampicillin, chloramphenicol, trimethoprim-sulfamethoxazole, amoxicillin, and ciprofloxacin), typhoid fever remains a big public health problem causing 11 million cases and 100,000 deaths a year, report the researchers in The Lancet Microbe.
In this study, Andrew and colleagues sequenced the genomes of 3489 S. Typhi strains collected during surveillance studies in Nepal, Bangladesh, Pakistan, and India between 2014 and 2019. They combined these new sequences with 4169 previously collected S. Typhi sequences collected between 1905 and 2018.
The team found that mutations in the quinolone-resistance determining region (QRDR) of S. Typhi have occurred and been spread on at least 94 occasions, nearly all in south Asia. Another mutation conferring resistance to azithromycin appeared in Bangladesh in 2013 and has been spreading since then.
Notably, according to the researchers, strains with multiple QRDR variants are becoming more common, some also including fluoroquinolone resistance, and are often outcompeting less resistant strains. The team found evidence to show resistant strains have been transferred between countries at least 138 times and between continents at least 59 times, following which they commonly out compete the local more drug susceptible strains.
“The results indicate that south Asia continues to be a crucial hub for S. Typhi antimicrobial resistance acquisition, and antimicrobial-resistant clones that emerge in this region have been regularly introduced across borders within the region and intercontinentally,” write the authors.
“Our analysis also suggests that multidrug-resistant strains are declining in most parts of south Asia but are being replaced with strains containing ceftriaxone resistance (extensively drug-resistant), high-level fluoroquinolone resistance, or azithromycin resistance, which are reversing declines in the effective population size of S. Typhi.”
The authors acknowledge that while this is one of the largest studies analyzing multiple S. Typhi genomes, there are a number of areas where typhoid is common that were not included, such as sub-Saharan Africa and Oceania. However, this analysis does give an important insight into current resistance trends and suggests more needs to be done to continue genomic surveillance of this dangerous pathogen.











