Scientists at Sanford Burnham Prebys Medical Discovery Institute, in collaboration with researchers at NYU Langone’s Perlmutter Cancer Center have identified a new potential strategy for boosting the immune system’s ability to fight cancer. Studies in gene knockout mice suggested that a protein known as Siah2 is involved in the control of T regulatory cells (Tregs) that limit the effectiveness of anticancer immunotherapies. The study findings indicate that targeting Siah2 may enhance the effectiveness of immune checkpoint inhibition using anti-PD-1 therapy, in cases where treatment would otherwise fail.
“While Siah2 is involved in control of activities that govern cancer development, this study offers the first direct evidence for its role in the immune system, namely in anti-tumor immunity,” commented Ze’ev Ronai, PhD, professor in Sanford Burnham Prebys’ Tumor Initiation and Maintenance Program, who is senior author of the study, which is published in Nature Communications. “Our study shows that a PD-1 inhibitor can be used to treat tumors that currently do not respond to this therapy, when administered in mice lacking the Siah2 gene, thereby offering a means to expand the effectiveness of immunotherapy. The findings also provide further justification for our efforts to find a drug that blocks Siah2.” Ronai and colleagues described their findings in a paper titled, “Siah2 control of T-regulatory cells limits anti-tumor immunity.”
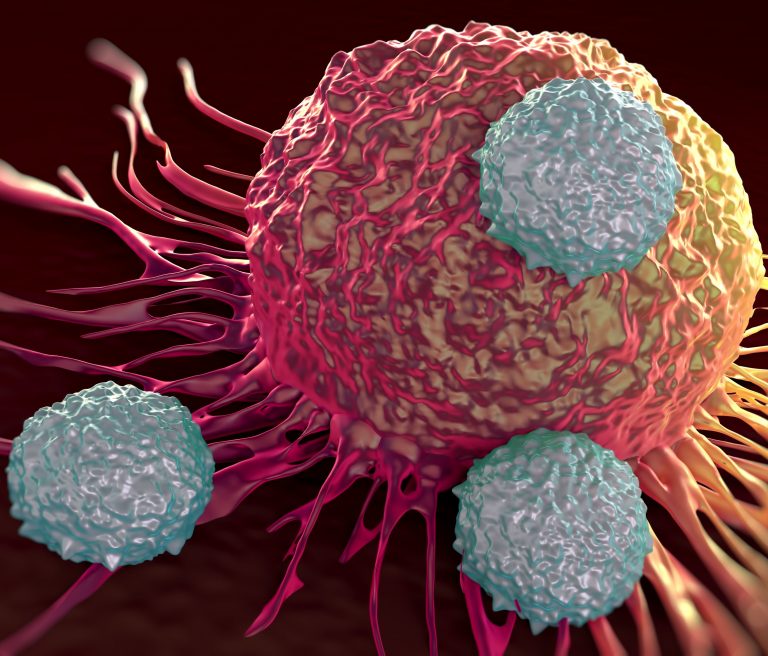
The development of immune checkpoint therapies (ICTs) that exploit the body’s own immune system against tumors has revolutionized the treatment of certain cancers over the last decade. For some people with advanced melanoma, such treatment has extended survival from months, to years. However, therapy is only effective in about 40% of people with advanced melanoma.
Scientists have long known that Siah2 is involved in the control of multiple fundamental cellular processes, including response to hypoxia (low oxygen) and the unfolded protein response, which are two mechanisms that tumors exploit for growth. Ronai has studied Siah2 for nearly a decade with a view to identifying improved cancer treatments, and his team is currently working to develop a small molecule drug that blocks the protein. But while the involvement of Siah2 in cancer-related cellular processes is well recognized, its direct involvement in the immune response to cancer hadn’t yet been demonstrated. “While these activities are associated with immune cell function, direct evidence for Siah2 regulation of anti-tumor immunity has been lacking,” the authors wrote.
Their newly reported study has now shown that Siah2 does play an important role in regulating the immune system’s response to a tumor, at least in mice. For their research, the scientists used genetically engineered animals that lack Siah2 protein (Siah2-/- mice) and into which they transferred BRAF-mutant melanomas. This type of mutation occurs in about half of human melanomas. The mouse model allowed the researchers to study the role of Siah2 in the tumor’s microenvironment, of which the immune system is a major component. They found that whereas in control mice that produced Siah2 the melanoma tumors grew readily, in animals lacking the Siah2 gene, the melanoma tumors receded. Treating Siah2-/- animals using anti-PD-1 therapy effectively eliminated melanoma that in control animals would resist treatment.
Further studies showed that tumors in the Siah2-/- mice were infiltrated by killer T cells but not Treg immune cells, which indicated that the immune system in these gene knockout animals were more active in clearing the tumors. The lack of Treg cells in the engineered mice was attributed to reduced proliferation and recruitment into the tumor because of the absence of Siah2 and its control of cell cycle regulatory proteins. “Here, using a genetic mouse model of global Siah2 deletion, we show that Siah2 functions in intratumoral recruitment and cell cycle control of T cells with the most notable impact on T regulatory cells (Tregs), supporting a function in anti-tumor immunity,” the authors wrote. “Our data points to changes in Treg proliferation, suppressive function, and recruitment which collectively impact their abundance in tumors, enabling enhanced anti-tumor immunity.”
As Ronai further explained, “In our study, mice lacking the Siah2 gene were able to mount an immune attack against melanoma. Moreover, the effectiveness of Siah2 in immunotherapy was demonstrated for ‘cold’ tumors—those that do not respond to immunotherapy—which were effectively eliminated by a PD-1 blockade in Siah2-mutant mice.” The authors suggested that their findings could have implications for CTLA4 therapy. “Limiting Treg infiltration or suppressive function is also expected to support CTLA4-based therapy, which does not impact this select immune cell population.”
“Understanding the basic mechanisms of tumor immunity will ultimately help us improve the effectiveness of immunotherapy,” commented Michael Rape, PhD, Howard Hughes investigator and professor of cell and developmental biology at the University of California, Berkeley. This study uncovers an important layer in the regulation of key immune cell components that impact the effectiveness of cancer immunotherapy, highlighting the need to develop inhibitors for Tregs, in which a Siah2 inhibitor holds promise.”
As the authors concluded, “Our data further supports the notion that combining ICT with cell cycle-disrupting drugs provides an effective strategy to promote an anti-tumor response. Targeting the ubiquitin ligase Siah2, central in cell autonomous proliferation and activity of Tregs, may thus offer the rationale for an innovative therapeutic approach.”
“Our discovery only fuels our sense of urgency to find a drug that inhibits Siah2,” stated Ronai. “Using an arsenal of novel approaches should enable us to advance the targeting of Siah2 in both the tumors and their microenvironment.”













