A new multi-center study has found that therapies which engage T cells such as bispecific antibodies and CAR-T cell therapies exhibit the most durable response in patients with relapsed or refractory multiple myeloma following BCMA-directed CAR-T cell therapy.
The study, published in the journal Blood, was led by Sham Mailankody, MBBS, medical oncologist and associate attending physician at Memorial Sloan Kettering Cancer Center, New York, and Samir Parekh, MD, director of translational research in multiple myeloma and co-leader of the cancer clinical investigation program at The Tisch Cancer Institute at the Icahn School of Medicine at Mount Sinai, New York.
“The findings of this study will serve as a benchmark for future prospective clinical studies that intend to improve the outcomes of patients who progress after CAR-T,” said Parekh. “This is the first study to report outcomes of different therapeutic options given to a large cohort of patients who relapsed after anti-BCMA CAR-T therapy. This is one of the most urgent and unmet needs in myeloma patients and, therefore, of great interest to the hematology community.”
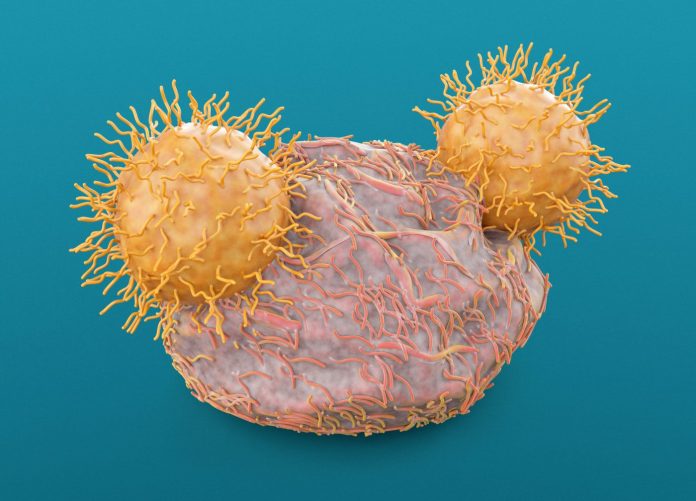
Multiple myeloma is a devastating form of blood cancer that affects antibody-producing, mature white blood cells called plasma cells in the bone marrow. Chimeric antigen receptor T-cell (CAR-T) immunotherapy that involves modifying the patient’s own immune T lymphocytes ex vivo and reinjecting them into the patient, has been very effective in treating patients with relapsed or intractable multiple myeloma—specifically, a CAR-T therapy that targets the B-cell maturation antigen (BCMA), a protein on cancerous plasma cells.
The U.S. Food and Drug Administration (FDA) has approved two BCMA-directed CAR-T cell therapies in relapsed or refractory multiple myeloma (RRMM) patients who have received at least three classes of drugs in earlier treatments (an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 antibody). RRMM patients who relapse after receiving BCMA-directed CAR-T cell therapy, however, have limited treatment options with no established guidelines for standard of care.
This retrospective study addresses this major gap in the effectiveness of immunotherapy. The researchers studied diseases characteristics, salvage treatments and outcomes in 79 RRMM patients in whom the disease had returned after BCMA-directed CAR-T cell therapy. Treatments given when a patient does not respond to standard therapy are called salvage or rescue treatments. The patients were treated at two institutions—The Tisch Cancer Institute and Memorial Sloan Kettering.
The researchers reported, the patients’ median overall survival (OS) from the date of relapse is about 18 months. The 79 RRMM patients received a total of 237 post-CAR-T salvage treatments with a median of two treatment lines. The overall response rate (ORR) to the first salvage treatment was 43.4%, with 44.3% patients receiving a T cell-engaging therapy (bispecific antibody or subsequent CAR T) as salvage treatment.
“We’re encouraged that subsequent use of other novel immune therapies like a second CAR-T cell therapy, or a bispecific antibody was feasible and led to durable responses in patients,” said Mailankody. “We look forward to continuing this work and unlocking the full potential of immune therapies for patients with multiple myeloma.”













